What is lupus belly

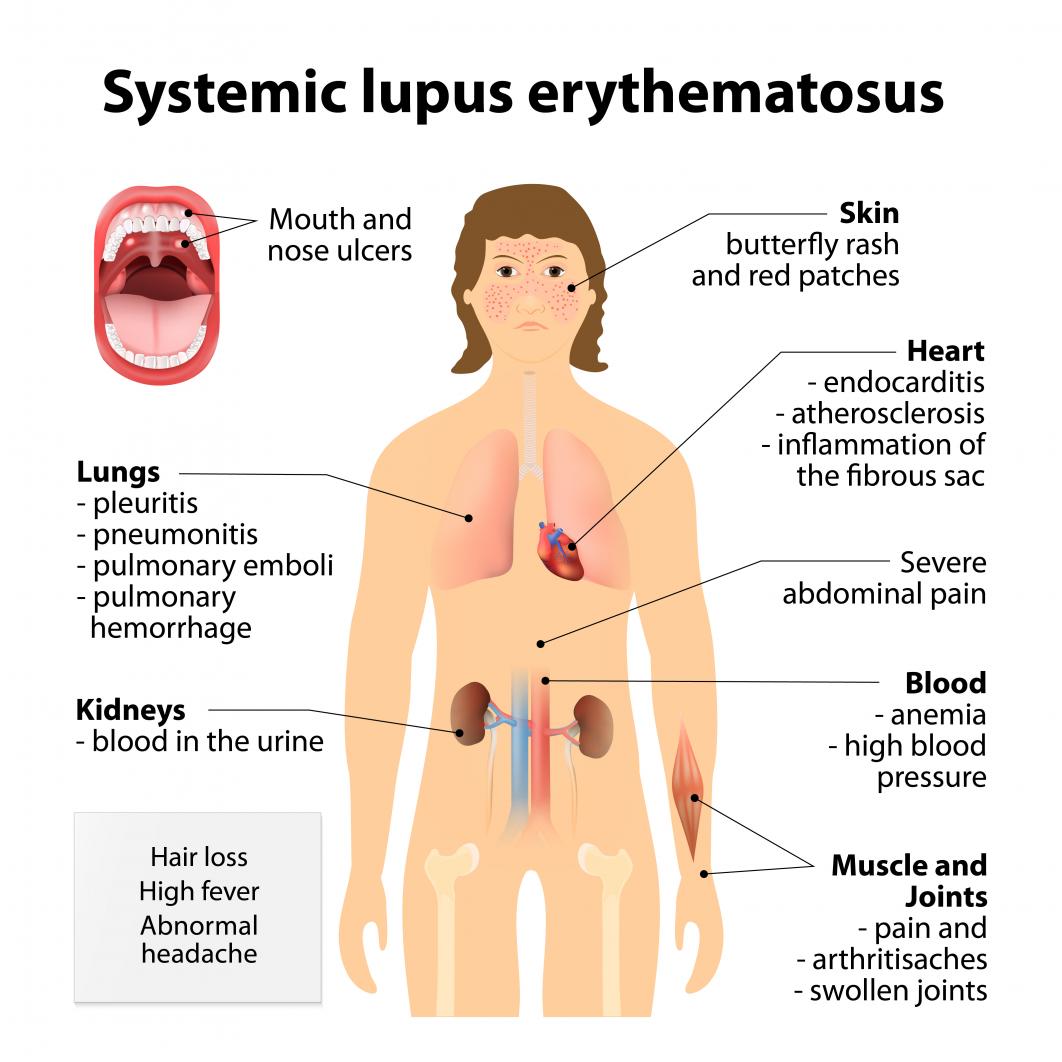
Lupus, a chronic autoimmune disease, can manifest in various ways, one of which is the development of a distinctive abdominal condition known as "lupus belly." This protrusion of the abdomen is a common symptom, but its underlying causes and implications often remain unclear. In this article, we delve into the complexities of lupus belly, exploring its characteristics, potential triggers, and the impact it can have on the overall health and well-being of individuals living with lupus.
What is Lupus Belly and its Manifestations?
Lupus belly, also known as lupus-related abdominal pain or abdominal manifestations of lupus, refers to a range of gastrointestinal symptoms experienced by individuals with systemic lupus erythematosus (SLE). It's not a distinct diagnosis in itself, but rather a collection of symptoms associated with the autoimmune disease. These symptoms can vary widely in severity and presentation, making diagnosis challenging. The abdominal pain and other digestive issues are often caused by inflammation associated with lupus, affecting various organs in the abdomen, such as the intestines, stomach, liver, and pancreas. The exact mechanisms that lead to these symptoms are not fully understood, but inflammation and immune system dysregulation play significant roles.
What causes abdominal pain in lupus?
The abdominal pain in lupus isn't directly caused by the lupus itself, but rather by the inflammation it triggers. This inflammation can affect various abdominal organs. For example, peritonitis (inflammation of the peritoneum, the lining of the abdominal cavity) can cause severe pain. Inflammation of the intestines can lead to cramping, diarrhea, and nausea. Lupus can also affect the blood vessels in the abdomen, potentially leading to vasculitis, which causes pain and other digestive problems. Additionally, lupus nephritis (kidney inflammation) can lead to abdominal discomfort. Finally, some lupus medications can also cause gastrointestinal side effects.
Other common digestive symptoms associated with lupus belly
Beyond abdominal pain, lupus can manifest in other digestive symptoms. These include nausea, vomiting, diarrhea, constipation, bloating, and indigestion. The frequency and severity of these symptoms vary widely among individuals. Some people experience mild discomfort, while others have debilitating symptoms that significantly impact their quality of life. The lack of specificity in these symptoms can make it difficult to definitively attribute them to lupus without considering other factors.
How is lupus belly diagnosed?
Diagnosing lupus belly is challenging due to the non-specific nature of the symptoms. There's no single test to confirm lupus belly. Instead, doctors rely on a combination of factors. This includes a thorough medical history, a physical examination focusing on the abdomen, and a review of other lupus symptoms. Blood tests to check for lupus-specific antibodies are crucial. Imaging studies, such as ultrasound or CT scans, may be used to rule out other causes of abdominal pain. A colonoscopy or endoscopy might be necessary in certain cases to evaluate the intestines and rule out other conditions. The diagnostic process often involves ruling out other potential causes of abdominal discomfort.
Treatment options for lupus belly
Treatment for lupus belly focuses on managing the underlying lupus and alleviating the gastrointestinal symptoms. This typically involves medication to control the autoimmune response, such as corticosteroids or immunosuppressants. Pain relievers can help manage abdominal pain. Dietary changes, such as avoiding trigger foods, can sometimes improve symptoms. In some cases, medications targeting specific gastrointestinal issues, such as anti-diarrheal or anti-nausea medications, may be necessary. The treatment approach is highly individualized and depends on the severity of the symptoms and the overall health of the patient.
Living with lupus belly: managing the condition
Living with lupus belly requires a proactive approach to managing symptoms and overall well-being. This involves close collaboration with a rheumatologist and potentially a gastroenterologist. Regular check-ups are essential to monitor disease activity and adjust treatment as needed. Lifestyle modifications, such as stress management techniques and a healthy diet, can play a significant role in improving symptoms. Support groups and counseling can also provide emotional support and practical strategies for coping with the challenges of managing this condition. It's important to remember that managing lupus belly is an ongoing process that requires patience and self-advocacy.
| Symptom | Possible Cause | Treatment Approach |
|---|---|---|
| Abdominal Pain | Inflammation of abdominal organs, vasculitis | Pain relievers, immunosuppressants |
| Nausea/Vomiting | Intestinal inflammation, medication side effects | Antiemetics, dietary adjustments |
| Diarrhea/Constipation | Intestinal dysmotility, medication side effects | Antidiarrheals, laxatives (as needed), dietary adjustments |
| Bloating | Intestinal inflammation, altered gut microbiota | Dietary changes, managing underlying inflammation |
What is Lupus Belly and its Manifestations?
Lupus belly, also known as lupus-related abdominal pain or abdominal manifestations of lupus, refers to a range of gastrointestinal symptoms experienced by individuals with systemic lupus erythematosus (SLE). It's not a distinct diagnosis in itself, but rather a collection of symptoms associated with the autoimmune disease. These symptoms can vary widely in severity and presentation, making diagnosis challenging. The abdominal pain and other digestive issues are often caused by inflammation associated with lupus, affecting various organs in the abdomen, such as the intestines, stomach, liver, and pancreas. The exact mechanisms that lead to these symptoms are not fully understood, but inflammation and immune system dysregulation play significant roles.
What causes abdominal pain in lupus?
The abdominal pain in lupus isn't directly caused by the lupus itself, but rather by the inflammation it triggers. This inflammation can affect various abdominal organs. For example, peritonitis (inflammation of the peritoneum, the lining of the abdominal cavity) can cause severe pain. Inflammation of the intestines can lead to cramping, diarrhea, and nausea. Lupus can also affect the blood vessels in the abdomen, potentially leading to vasculitis, which causes pain and other digestive problems. Additionally, lupus nephritis (kidney inflammation) can lead to abdominal discomfort. Finally, some lupus medications can also cause gastrointestinal side effects.
Other common digestive symptoms associated with lupus belly
Beyond abdominal pain, lupus can manifest in other digestive symptoms. These include nausea, vomiting, diarrhea, constipation, bloating, and indigestion. The frequency and severity of these symptoms vary widely among individuals. Some people experience mild discomfort, while others have debilitating symptoms that significantly impact their quality of life. The lack of specificity in these symptoms can make it difficult to definitively attribute them to lupus without considering other factors.
How is lupus belly diagnosed?
Diagnosing lupus belly is challenging due to the non-specific nature of the symptoms. There's no single test to confirm lupus belly. Instead, doctors rely on a combination of factors. This includes a thorough medical history, a physical examination focusing on the abdomen, and a review of other lupus symptoms. Blood tests to check for lupus-specific antibodies are crucial. Imaging studies, such as ultrasound or CT scans, may be used to rule out other causes of abdominal pain. A colonoscopy or endoscopy might be necessary in certain cases to evaluate the intestines and rule out other conditions. The diagnostic process often involves ruling out other potential causes of abdominal discomfort.
Treatment options for lupus belly
Treatment for lupus belly focuses on managing the underlying lupus and alleviating the gastrointestinal symptoms. This typically involves medication to control the autoimmune response, such as corticosteroids or immunosuppressants. Pain relievers can help manage abdominal pain. Dietary changes, such as avoiding trigger foods, can sometimes improve symptoms. In some cases, medications targeting specific gastrointestinal issues, such as anti-diarrheal or anti-nausea medications, may be necessary. The treatment approach is highly individualized and depends on the severity of the symptoms and the overall health of the patient.
Living with lupus belly: managing the condition
Living with lupus belly requires a proactive approach to managing symptoms and overall well-being. This involves close collaboration with a rheumatologist and potentially a gastroenterologist. Regular check-ups are essential to monitor disease activity and adjust treatment as needed. Lifestyle modifications, such as stress management techniques and a healthy diet, can play a significant role in improving symptoms. Support groups and counseling can also provide emotional support and practical strategies for coping with the challenges of managing this condition. It's important to remember that managing lupus belly is an ongoing process that requires patience and self-advocacy.
| Symptom | Possible Cause | Treatment Approach |
|---|---|---|
| Abdominal Pain | Inflammation of abdominal organs, vasculitis | Pain relievers, immunosuppressants |
| Nausea/Vomiting | Intestinal inflammation, medication side effects | Antiemetics, dietary adjustments |
| Diarrhea/Constipation | Intestinal dysmotility, medication side effects | Antidiarrheals, laxatives (as needed), dietary adjustments |
| Bloating | Intestinal inflammation, altered gut microbiota | Dietary changes, managing underlying inflammation |
What are the symptoms of lupus in the stomach?

Lupus is a systemic autoimmune disease that can affect many parts of the body, including the gastrointestinal tract. Symptoms in the stomach can vary widely in severity and presentation, making diagnosis challenging. They are often non-specific, meaning they can be caused by other conditions as well. It's crucial to consult a doctor for proper diagnosis if you suspect lupus-related stomach issues.
Gastrointestinal Upset and Pain
One of the most common manifestations of lupus in the stomach is general gastrointestinal discomfort. This can range from mild indigestion and bloating to more severe abdominal pain. The pain may be localized to a specific area or more diffuse throughout the abdomen. The intensity can fluctuate, sometimes being mild and intermittent, other times severe and persistent. It's important to note that this pain is often not directly related to food intake.
- Abdominal pain: ranging from mild cramping to severe, sharp pain.
- Indigestion and heartburn: frequent discomfort after eating.
- Bloating and gas: feelings of fullness and discomfort in the abdomen.
Nausea and Vomiting
Nausea and vomiting are frequent symptoms experienced by individuals with lupus affecting the stomach. These symptoms can be related to the inflammation and irritation in the gastrointestinal tract. The severity can range from mild queasiness to severe, projectile vomiting, impacting nutritional intake and overall health. The frequency of these episodes also varies greatly.
- Nausea: feeling sick to the stomach.
- Vomiting: forceful expulsion of stomach contents.
- Loss of appetite: decreased desire to eat, leading to weight loss.
Changes in Bowel Habits
Lupus can also impact bowel function, leading to alterations in bowel habits. These changes can manifest as diarrhea, constipation, or both. The inflammation associated with lupus can affect the motility of the intestines, leading to inconsistent bowel movements. The frequency and consistency of stools should be carefully monitored.
- Diarrhea: loose, watery stools, often multiple times a day.
- Constipation: infrequent or difficult bowel movements.
- Changes in stool consistency: alterations in the firmness or appearance of feces.
Peptic Ulcers
In some cases, lupus can increase the risk of developing peptic ulcers, which are sores in the lining of the stomach or duodenum (the first part of the small intestine). These ulcers can be very painful and lead to complications such as bleeding. Risk factors for peptic ulcers include NSAID use, which is sometimes necessary to manage lupus symptoms.
- Severe stomach pain: often described as a burning sensation.
- Nausea and vomiting: especially after eating.
- Blood in vomit or stool: a sign of a serious complication.
Gastrointestinal Bleeding
Though less common, gastrointestinal bleeding can be a serious complication of lupus affecting the stomach. This can range from minor bleeding, only detectable through stool testing, to more severe bleeding requiring medical intervention. Symptoms can include dark, tarry stools or bright red blood in the stool or vomit. This is a medical emergency requiring immediate attention.
- Melena: dark, tarry stools due to digested blood.
- Hematochezia: bright red blood in the stool.
- Hematemesis: vomiting blood.
What does lupus hair look like?

There isn't a single, definitive "lupus hair look." Hair loss in lupus is highly variable, depending on the type of lupus, the severity of the disease, and the individual's response to treatment. It's not a diagnostic feature, meaning doctors don't diagnose lupus based on hair loss alone. Instead, hair loss is often a symptom that appears alongside other characteristic signs and symptoms. The hair loss can range from mild thinning to significant patches of hair loss, and it can affect the scalp and/or other areas of the body.
Types of Hair Loss Associated with Lupus
Lupus can cause various types of hair loss. The most common is telogen effluvium, a diffuse thinning of hair across the scalp. This occurs because the disease disrupts the hair growth cycle, causing more hairs to enter the resting phase (telogen) and shed prematurely. This type of hair loss is often reversible with treatment. Another, more noticeable form of hair loss is alopecia areata, which manifests as round or oval patches of hair loss. This is an autoimmune condition where the immune system attacks the hair follicles, and it's possible to have alopecia areata in conjunction with lupus. Finally, some individuals with lupus may experience scarring alopecia, a type of permanent hair loss caused by damage or destruction of hair follicles. This is less common in lupus but can be a serious complication.
- Telogen effluvium: Diffuse thinning, often reversible.
- Alopecia areata: Round or oval patches of hair loss.
- Scarring alopecia: Permanent hair loss due to follicle damage.
The Role of Medications
The medications used to treat lupus can also contribute to hair loss. Some immunosuppressants, such as methotrexate and cyclophosphamide, are known to cause hair thinning or shedding as a side effect. This type of hair loss is usually temporary and often improves once the medication is stopped or the dosage is adjusted. It's crucial to discuss any concerns about hair loss with your doctor to determine the cause and potential management strategies. They can help differentiate between hair loss caused directly by lupus and that caused by lupus medications.
- Immunosuppressants can cause temporary hair loss as a side effect.
- Dosage adjustments or medication changes may be considered.
- Open communication with your doctor is vital for managing medication-related hair loss.
Hair Texture and Appearance Changes
Beyond simply losing hair, individuals with lupus might also experience changes in hair texture and appearance. This can include hair that is brittle, dry, or easily broken. This can be related to the inflammation associated with lupus, impacting the overall health of the hair shaft. In addition, the stress associated with managing a chronic illness like lupus can also negatively impact hair health, exacerbating existing hair loss or contributing to new issues. Proper hair care, avoiding harsh chemicals, and maintaining a healthy diet can be helpful in mitigating some of these symptoms.
- Hair may become brittle, dry, and prone to breakage.
- Stress related to lupus can worsen hair health.
- Gentle hair care practices and a healthy lifestyle can help.
The Importance of Diagnosis
It's crucial to remember that hair loss alone isn't diagnostic of lupus. Many other conditions can cause hair loss. A proper diagnosis of lupus requires a comprehensive evaluation by a doctor, involving a review of symptoms, medical history, and potentially blood tests and other diagnostic procedures. Don't self-diagnose based on hair loss. If you are experiencing hair loss along with other symptoms such as fatigue, joint pain, skin rashes, or fever, it's important to seek medical attention to determine the underlying cause.
- Hair loss is not a definitive sign of lupus; it's often a symptom among many.
- A doctor's diagnosis is necessary for accurate identification.
- Seek medical advice if experiencing hair loss combined with other symptoms.
Managing Hair Loss in Lupus
Managing hair loss related to lupus often involves addressing the underlying lupus itself. Treatment strategies focus on controlling inflammation and suppressing the autoimmune response. This might involve medications like corticosteroids, immunosuppressants, or biologics. In addition to medical management, lifestyle factors play a crucial role. Maintaining a healthy diet, managing stress levels, and using gentle hair care products can all help to support hair health and minimize further damage. Some individuals also find that using gentle hair care products, avoiding harsh chemicals, and protecting their hair from sun damage can make a difference.
- Treating the underlying lupus is key to managing hair loss.
- Lifestyle modifications, including diet and stress management, are important.
- Gentle hair care practices can help minimize further damage.
What is the biggest symptom of lupus?
There is no single "biggest" symptom of lupus because it's a systemic autoimmune disease that can affect many different parts of the body, manifesting in a wide array of symptoms. The severity and combination of symptoms vary greatly from person to person. However, fatigue is frequently cited as one of the most common and debilitating symptoms, often impacting daily life significantly more than other symptoms.
Fatigue in Lupus
Fatigue in lupus is not simply tiredness; it's a profound and persistent exhaustion that doesn't improve with rest. It can interfere with work, social activities, and even basic daily tasks. This overwhelming tiredness is often one of the first symptoms to appear and can persist throughout the course of the disease. It's crucial to distinguish lupus fatigue from typical tiredness as it significantly impacts quality of life.
- Intense tiredness that doesn't improve with sleep.
- Difficulty concentrating and remembering things (brain fog).
- Reduced physical endurance and stamina.
Joint Pain (Arthralgia) and Inflammation (Arthritis)
Many individuals with lupus experience joint pain and swelling, commonly affecting the hands, wrists, knees, and ankles. This inflammation can be significant, causing stiffness, limited range of motion, and discomfort. While not always the most prominent symptom, the chronic nature of joint pain significantly impacts daily activities and overall well-being. The severity can fluctuate, sometimes causing periods of significant disability.
- Pain and swelling in joints.
- Joint stiffness, particularly in the morning.
- Limited range of motion and difficulty with movement.
Skin Rash (Malar Rash or Butterfly Rash)
A characteristic skin manifestation of lupus is the malar rash, often described as a "butterfly rash" because of its symmetrical appearance across the cheeks and bridge of the nose. While not everyone with lupus develops this rash, its presence can be a strong indicator. This rash can be sensitive to sunlight and may worsen with sun exposure. Other skin manifestations, such as discoid lupus (raised, scaly patches), are also common.
- Red, raised rash on the face, particularly across the cheeks and nose.
- Sensitivity to sunlight (photosensitivity).
- Scaly or discolored skin patches (discoid lupus).
Fever
Low-grade fever is a common symptom of lupus, often appearing without any other obvious infection. This fever can be intermittent and unpredictable, making it difficult to diagnose and manage. The unexplained fever, alongside other lupus symptoms, can be a significant indicator of disease activity. It often accompanies periods of inflammation and disease flares.
- Low-grade fever (often below 101°F or 38.3°C).
- Intermittent fever that comes and goes.
- Fever without any other signs of infection.
Raynaud's Phenomenon
Raynaud's phenomenon is a condition that affects the blood vessels in the extremities (fingers and toes). In response to cold temperatures or stress, the blood vessels constrict, causing the fingers and toes to turn white or blue, and then red as blood flow returns. This can cause numbness, tingling, and pain. It's a common symptom of lupus, and its presence can be an early indicator of the disease.
- Color changes in fingers and toes (white, blue, then red).
- Numbness and tingling in the extremities.
- Pain in the fingers and toes, often triggered by cold or stress.
Does lupus cause belly fat?

Lupus itself doesn't directly cause belly fat. However, several factors associated with lupus can contribute to weight gain, including abdominal fat accumulation. The medications used to treat lupus, lifestyle changes necessitated by the disease, and the disease's impact on metabolism can all play a role. It's crucial to understand that weight gain in lupus patients is often a complex issue with multiple contributing factors, rather than a direct causal effect of the autoimmune disease itself. This means that the relationship between lupus and belly fat is indirect and multifaceted rather than a simple cause-and-effect relationship.
Medication Side Effects
Many medications used to treat lupus, such as corticosteroids (like prednisone), can cause significant weight gain, often concentrated in the abdominal area. This is due to several mechanisms, including increased appetite, fluid retention, and changes in fat distribution. The weight gain can be substantial and challenging to manage, even with dietary changes and exercise. It's important to discuss any weight concerns with your doctor, as they may be able to adjust your medication or suggest strategies for managing weight gain.
- Corticosteroids are potent anti-inflammatory drugs that are often essential in lupus treatment, but they frequently lead to increased appetite and weight gain.
- Immunosuppressants, while vital for managing lupus symptoms, can also impact metabolism and contribute to weight changes.
- Some other medications used to treat lupus symptoms or its complications may have weight gain as a side effect.
Lifestyle Changes Due to Lupus
Living with lupus can lead to lifestyle changes that unintentionally contribute to weight gain. Fatigue, pain, and reduced mobility often make it difficult to engage in regular physical activity, a crucial factor in maintaining a healthy weight. Moreover, the emotional distress and stress associated with managing a chronic illness can lead to changes in eating habits, potentially contributing to weight gain.
- Reduced physical activity: Fatigue and pain associated with lupus often make exercise challenging, leading to reduced calorie expenditure.
- Changes in appetite and eating habits: Stress and the need for comfort may lead to increased food consumption.
- Difficulty with daily activities: Lupus can significantly impact daily activities and make it hard to maintain healthy habits.
Metabolic Changes in Lupus
Lupus can affect the body's metabolism, potentially leading to weight changes. Inflammation, a hallmark of lupus, can disrupt metabolic processes, contributing to increased fat storage and weight gain. Additionally, hormonal imbalances associated with lupus can also affect metabolism and influence weight.
- Chronic inflammation disrupts normal metabolic function, potentially promoting fat storage.
- Hormonal imbalances, common in lupus, can alter metabolism and influence body composition.
- Changes in insulin sensitivity can lead to impaired glucose metabolism and weight gain.
Inflammation and Fat Distribution
The chronic inflammation characteristic of lupus can alter the body's distribution of fat, resulting in an increase in visceral fat (fat around the organs), which is often associated with abdominal obesity. This type of fat is particularly harmful to health, contributing to an increased risk of cardiovascular disease and other complications.
- Visceral fat accumulation: Inflammation may lead to increased storage of visceral fat, a particularly unhealthy type of fat.
- Increased risk of cardiovascular disease: Visceral fat is strongly linked to an increased risk of heart disease.
- Impact on metabolic syndrome: Abdominal obesity can contribute to the development of metabolic syndrome, a cluster of conditions that increase the risk of various health problems.
Importance of Consulting a Doctor
If you are experiencing weight gain while managing lupus, it's crucial to consult your doctor. They can assess your specific situation, consider the various factors contributing to your weight gain, and develop a personalized management plan. This may involve adjusting medications, lifestyle modifications, dietary changes, and possibly referral to specialists like a dietitian or physical therapist. Early intervention is crucial to mitigate the health risks associated with weight gain and maintain overall well-being.
- Personalized management plan: Your doctor can create a plan tailored to your specific needs and circumstances.
- Medication adjustments: Your medication regimen may be adjusted to minimize weight gain as a side effect.
- Lifestyle modifications and dietary advice: Your doctor may recommend changes in your diet and activity levels.
What exactly is "lupus belly"?
“Lupus belly,” or more accurately, abdominal involvement in lupus, isn't a formally recognized medical term. It's a colloquialism used to describe the various abdominal symptoms and complications that can arise in individuals with systemic lupus erythematosus (SLE). SLE is an autoimmune disease where the body's immune system mistakenly attacks its own tissues and organs. While lupus can affect virtually any part of the body, the abdomen is frequently involved. The symptoms are diverse and can range from mild discomfort to severe, debilitating conditions. These symptoms aren't always directly caused by lupus attacking the abdominal organs themselves, but can be secondary effects or manifestations of the disease. For example, inflammation in other parts of the body, common in lupus, can lead to secondary abdominal issues. Peritoneal inflammation, a complication of lupus, can cause significant abdominal pain and distension. Lupus can also lead to kidney problems (lupus nephritis), which may manifest as abdominal pain or swelling. Furthermore, the medications used to treat lupus can have gastrointestinal side effects, adding to the complexity of abdominal symptoms. Therefore, "lupus belly" encompasses a broad spectrum of abdominal manifestations connected to the disease, rather than a specific diagnosis.
What are the common symptoms of abdominal involvement in lupus?
The symptoms associated with abdominal involvement in lupus are highly variable and depend on the specific organs and systems affected. Abdominal pain is a frequent complaint, ranging from mild discomfort to severe, debilitating cramps. This pain can be localized or diffuse, and its intensity can fluctuate. Swelling (ascites) in the abdomen is another common symptom, often resulting from inflammation or fluid buildup. Bloating and distension are also frequently experienced, often accompanied by feelings of fullness even after small meals. Gastrointestinal issues such as nausea, vomiting, diarrhea, or constipation are common occurrences. These issues can be caused by the direct effects of lupus on the gastrointestinal tract, medication side effects, or secondary effects of inflammation elsewhere in the body. Less common but potentially serious symptoms include intestinal inflammation and peritonitis, a severe inflammation of the lining of the abdominal cavity. In some cases, lupus can also affect the liver, pancreas, and spleen, resulting in additional abdominal symptoms related to those organs' specific functions. The presence and severity of these symptoms vary significantly between individuals with lupus, highlighting the importance of individual assessment and tailored treatment plans.
How is abdominal involvement in lupus diagnosed?
Diagnosing abdominal involvement in lupus can be challenging because the symptoms are often nonspecific and can mimic other conditions. A thorough medical history, including a detailed account of the patient's symptoms, is the first step. The physician will consider the patient's overall lupus diagnosis and symptoms. Physical examination of the abdomen is crucial, paying attention to areas of tenderness, swelling, and distension. Imaging tests, such as ultrasound, CT scans, and MRI, can help visualize abdominal organs and detect abnormalities like ascites or inflammation. Blood tests are essential to assess markers of inflammation and organ damage, including kidney function tests and liver function tests. Biopsies might be necessary to confirm the diagnosis of specific complications such as inflammation of the peritoneum or intestines. It's crucial to rule out other potential causes of the abdominal symptoms, such as infections, inflammatory bowel disease, or other gastrointestinal disorders. Because the presentation can be varied and challenging, accurate diagnosis often requires a collaborative approach involving specialists like rheumatologists, gastroenterologists, and nephrologists, especially when dealing with complications affecting multiple organs.
How is abdominal involvement in lupus treated?
Treatment for abdominal involvement in lupus depends on the specific cause and severity of the symptoms. Managing the underlying lupus is paramount; this typically involves medications to suppress the immune system, such as corticosteroids, immunosuppressants, and biologics. If there's significant inflammation, anti-inflammatory medications like NSAIDs (nonsteroidal anti-inflammatory drugs) might be used, but with caution given their potential side effects on the gastrointestinal tract. Symptomatic treatment focuses on relieving the individual's discomfort. This may include pain relievers, anti-diarrheal or anti-constipation medications, and dietary modifications. In cases of significant fluid buildup (ascites), paracentesis (a procedure to drain fluid from the abdomen) might be necessary. For severe complications like peritonitis or intestinal inflammation, hospitalization and more aggressive medical interventions may be required. Dietary adjustments can play a crucial role, especially in managing digestive issues. A balanced diet that's easy to digest, alongside avoiding known triggers, can significantly improve symptoms. Regular monitoring of organ function and disease activity is essential to ensure treatment effectiveness and to make timely adjustments to the management strategy. It's crucial to work closely with a medical team experienced in managing lupus to develop a personalized treatment plan that addresses the individual's specific needs and symptoms.
Deja una respuesta