What is the leading cause of mouth sores

Mouth sores, also known as aphthous ulcers, are a common and often painful oral condition that can affect people of all ages. While there are many potential causes of mouth sores, the most common is a minor injury to the mouth's soft tissues. This can occur through a variety of activities, such as biting the cheek or accidentally brushing too hard with a toothbrush. Other common causes of mouth sores include stress, hormonal changes, certain medications, and certain medical conditions. In most cases, mouth sores are harmless and will resolve on their own within a few weeks. However, in some cases, they may be a sign of a more serious underlying condition, and it is important to see a doctor if the sores are severe, persistent, or accompanied by other symptoms.
What is the Leading Cause of Mouth Sores?
While there isn't one single leading cause of mouth sores (also known as oral ulcers or canker sores), aphthous ulcers are the most common type. These are small, shallow lesions that typically appear on the inside of the cheeks, lips, tongue, or the floor of the mouth. However, various factors can contribute to their development, making pinpointing a single "leading cause" difficult.
Minor Trauma
Minor trauma to the mouth is a frequent culprit. This could include biting your cheek accidentally, accidentally brushing too hard, or even the irritation from poorly fitting dentures or braces. The injury triggers an inflammatory response, leading to the formation of a canker sore. The exact mechanism isn't fully understood, but the trauma likely disrupts the delicate mucosal lining of the mouth.
Stress
Stress is strongly linked to the occurrence of mouth sores. While the precise connection isn't entirely clear, it's believed that stress weakens the immune system, making individuals more susceptible to infections and inflammation, including the development of aphthous ulcers. Managing stress through techniques like exercise, meditation, or yoga may help reduce the frequency and severity of outbreaks.
Nutritional Deficiencies
Nutritional deficiencies, particularly in vitamins like B12, B6, folic acid, and iron, can increase the likelihood of developing mouth sores. These vitamins play crucial roles in maintaining healthy tissues and immune function. A balanced diet rich in fruits, vegetables, and whole grains is essential for preventing deficiencies and promoting oral health. If you suspect a deficiency, consult a doctor for testing and advice.
Immune System Issues
Problems with the immune system can also play a role. Conditions such as autoimmune diseases or weakened immunity due to illness or medication can make a person more prone to developing mouth sores. The immune system's response to even minor irritations may be exaggerated, leading to the formation of ulcers.
Certain Medications
Some medications, particularly those that affect the immune system or cause dry mouth, can increase the risk of mouth sores as a side effect. Nonsteroidal anti-inflammatory drugs (NSAIDs) and certain chemotherapy drugs are examples. If you suspect a medication is causing your mouth sores, consult your doctor or pharmacist to explore alternative options or management strategies.
| Cause | Description | Management |
|---|---|---|
| Minor Trauma | Accidental injury to the mouth's lining. | Gentle care, avoiding irritants. |
| Stress | Weakened immune response due to stress. | Stress management techniques (exercise, meditation). |
| Nutritional Deficiencies | Lack of essential vitamins and minerals. | Balanced diet, potential supplementation (under medical guidance). |
| Immune System Issues | Autoimmune diseases or weakened immunity. | Medical management of underlying condition. |
| Medications | Side effect of certain medications. | Consult doctor for alternative medication or management strategies. |
What is the Leading Cause of Mouth Sores?
While there isn't one single leading cause of mouth sores (also known as oral ulcers or canker sores), aphthous ulcers are the most common type. These are small, shallow lesions that typically appear on the inside of the cheeks, lips, tongue, or the floor of the mouth. However, various factors can contribute to their development, making pinpointing a single "leading cause" difficult.
Minor Trauma
Minor trauma to the mouth is a frequent culprit. This could include biting your cheek accidentally, accidentally brushing too hard, or even the irritation from poorly fitting dentures or braces. The injury triggers an inflammatory response, leading to the formation of a canker sore. The exact mechanism isn't fully understood, but the trauma likely disrupts the delicate mucosal lining of the mouth.
Stress
Stress is strongly linked to the occurrence of mouth sores. While the precise connection isn't entirely clear, it's believed that stress weakens the immune system, making individuals more susceptible to infections and inflammation, including the development of aphthous ulcers. Managing stress through techniques like exercise, meditation, or yoga may help reduce the frequency and severity of outbreaks.
Nutritional Deficiencies
Nutritional deficiencies, particularly in vitamins like B12, B6, folic acid, and iron, can increase the likelihood of developing mouth sores. These vitamins play crucial roles in maintaining healthy tissues and immune function. A balanced diet rich in fruits, vegetables, and whole grains is essential for preventing deficiencies and promoting oral health. If you suspect a deficiency, consult a doctor for testing and advice.
Immune System Issues
Problems with the immune system can also play a role. Conditions such as autoimmune diseases or weakened immunity due to illness or medication can make a person more prone to developing mouth sores. The immune system's response to even minor irritations may be exaggerated, leading to the formation of ulcers.
Certain Medications
Some medications, particularly those that affect the immune system or cause dry mouth, can increase the risk of mouth sores as a side effect. Nonsteroidal anti-inflammatory drugs (NSAIDs) and certain chemotherapy drugs are examples. If you suspect a medication is causing your mouth sores, consult your doctor or pharmacist to explore alternative options or management strategies.
| Cause | Description | Management |
|---|---|---|
| Minor Trauma | Accidental injury to the mouth's lining. | Gentle care, avoiding irritants. |
| Stress | Weakened immune response due to stress. | Stress management techniques (exercise, meditation). |
| Nutritional Deficiencies | Lack of essential vitamins and minerals. | Balanced diet, potential supplementation (under medical guidance). |
| Immune System Issues | Autoimmune diseases or weakened immunity. | Medical management of underlying condition. |
| Medications | Side effect of certain medications. | Consult doctor for alternative medication or management strategies. |
What is the main cause of mouth sores?
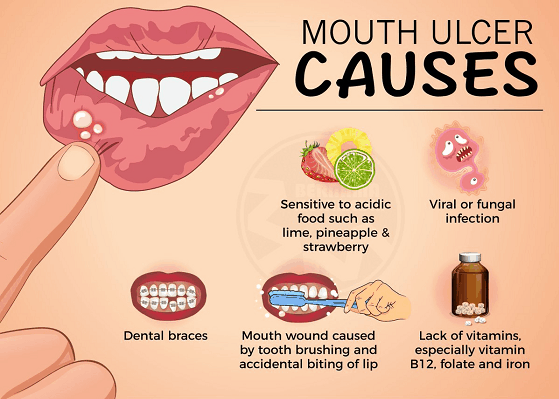
There isn't one single main cause of mouth sores (also known as mouth ulcers or aphthous ulcers). The exact cause is often unknown, but several factors are strongly implicated in their development. Stress, minor trauma, and nutritional deficiencies are frequently cited as contributing factors. However, in many cases, the triggering event remains elusive, and the sores resolve spontaneously. It's important to differentiate between canker sores (aphthous ulcers) and other mouth lesions, as the causes can vary significantly. For instance, cold sores (caused by the herpes simplex virus) are distinctly different and require separate treatment.
Viral Infections
While not always the maincause of all mouth sores, viral infections, particularly the herpes simplex virus (HSV), are a significant cause of certain types of mouth sores. HSV-1 is responsible for cold sores or fever blisters, which are typically found on the lips and surrounding areas. These sores are highly contagious and characterized by small, fluid-filled blisters. Proper hygiene and antiviral medication may help manage these outbreaks. Other viruses can also contribute to mouth sores, but HSV is among the most common and well-known.
- Herpes simplex virus (HSV-1) is the most common viral cause of mouth sores.
- Viral infections can cause painful blisters and ulcers.
- Antiviral medication can often reduce the duration and severity of viral mouth sores.
Minor Trauma
Accidental biting, dental work, or even vigorous brushing can sometimes cause minor trauma to the soft tissues in the mouth, resulting in the formation of mouth sores. These sores typically heal within a week or two without any specific treatment. However, repeated trauma or persistent irritation can lead to recurrent sores. Avoiding irritating foods and using a soft-bristled toothbrush can help prevent trauma-induced mouth sores.
- Accidental biting of the cheek or lip is a frequent cause.
- Poorly fitting dentures can also cause irritation and sores.
- Gentle brushing techniques can help prevent trauma.
Nutritional Deficiencies
Although not definitively proven as a primarycause for all, deficiencies in certain vitamins and minerals, such as vitamin B12, iron, and folate, have been associated with an increased risk of developing mouth sores. Maintaining a balanced diet rich in these nutrients can help reduce the likelihood of developing these sores. However, it's important to note that nutritional deficiencies are often one factor among many, and a deficiency alone does not guarantee the appearance of mouth sores. Regular blood tests can identify any nutritional deficiencies, allowing for appropriate supplementation if needed.
- Vitamin B12 deficiency is often linked to mouth sores.
- Iron deficiency can also contribute to the formation of mouth sores.
- A balanced diet is crucial for preventing nutrient deficiencies.
Stress
Stress is a widely recognized trigger for many people who experience recurring mouth sores. The exact mechanism isn't fully understood, but the link between stress and the immune system is well-established. Chronic stress can weaken the immune response, potentially making individuals more susceptible to mouth sores. Managing stress through techniques such as exercise, yoga, or meditation may help reduce the frequency and severity of these sores.
- Stress weakens the immune system.
- Chronic stress is a potential trigger for recurrent mouth sores.
- Stress management techniques can be helpful in reducing occurrences.
Underlying Medical Conditions
In some cases, mouth sores can be a symptom of an underlying medical condition, such as Behçet's disease, Crohn's disease, or celiac disease. These conditions often involve inflammation throughout the body. If mouth sores are severe, persistent, or accompanied by other symptoms, it's essential to consult a doctor to rule out any underlying medical issues. Diagnosis and treatment of the underlying condition may be necessary to effectively manage the mouth sores.
- Behçet's disease can manifest with recurrent mouth sores.
- Crohn's disease and other inflammatory bowel diseases can also be associated with mouth sores.
- Consult a doctor if mouth sores are severe, persistent, or accompanied by other symptoms.
What deficiency causes mouth sores?

Mouth sores, also known as aphthous ulcers or canker sores, can be caused by a variety of factors, but several nutritional deficiencies are strongly linked to their development. While a single deficiency rarely acts in isolation, these deficiencies often work synergistically to contribute to the formation of mouth sores. The most common nutritional deficiencies associated with mouth sores include iron, vitamin B12, folate, zinc, and riboflavin deficiencies. A deficiency in any of these vitamins and minerals can weaken the immune system and the integrity of the oral mucosa, making the mouth more susceptible to injury and inflammation leading to sores. Other factors such as stress, trauma, hormonal changes and certain medications can also play a role. It's important to note that the presence of mouth sores does not always indicate a deficiency; a doctor should always be consulted for proper diagnosis and treatment.
Iron Deficiency and Mouth Sores
Iron is crucial for the production of red blood cells, which carry oxygen throughout the body. Iron deficiency anemia can lead to a weakened immune system, making individuals more prone to infections and inflammation, including mouth sores. The lack of oxygen-carrying capacity also contributes to the compromised healing process. Symptoms beyond mouth sores might include fatigue, pallor, shortness of breath, and headaches.
- Reduced Oxygen Delivery: Insufficient iron reduces the oxygen-carrying capacity of the blood, hindering tissue repair and increasing susceptibility to mouth sores.
- Weakened Immune Response: Iron plays a crucial role in immune function. Deficiency can leave the body vulnerable to infections, including those that might trigger mouth sores.
- Delayed Wound Healing: The healing process requires adequate oxygen and nutrients. Iron deficiency impedes both, delaying the healing of mouth sores.
Vitamin B12 Deficiency and Mouth Sores
Vitamin B12 is essential for the production of red blood cells and the proper functioning of the nervous system. A deficiency in B12, often associated with pernicious anemia, can manifest as mouth sores due to its role in cell growth and repair. Other symptoms can include fatigue, weakness, numbness, tingling in the extremities, and memory problems.
- Impaired Cell Growth: Vitamin B12 is vital for the growth and repair of cells, including those lining the mouth. Deficiency leads to impaired healing.
- Neurological Symptoms: While less directly related to mouth sores, B12 deficiency’s impact on the nervous system can indirectly influence the body's response to injury and inflammation in the mouth.
- Anemia: B12 deficiency causes anemia, mirroring the effects of iron deficiency and contributing to a weakened immune response.
Folate Deficiency and Mouth Sores
Folate, also known as vitamin B9, is essential for DNA synthesis and cell division. Folate deficiency can impede cell growth and repair, potentially leading to mouth sores, alongside other symptoms like fatigue, weakness, and pale skin. Severe deficiency can cause megaloblastic anemia.
- Impaired Cell Regeneration: Folate is crucial for the rapid cell turnover in the mouth. Deficiency can slow down the regeneration of damaged cells, resulting in persistent sores.
- Weakened Immune System: Similar to other deficiencies, folate deficiency compromises immune function, increasing the susceptibility to infections that can exacerbate mouth sores.
- Megaloblastic Anemia: Severe folate deficiency can lead to megaloblastic anemia, a type of anemia characterized by abnormally large red blood cells.
Zinc Deficiency and Mouth Sores
Zinc plays a vital role in immune function, wound healing, and cell growth. Zinc deficiency weakens the immune system, impairing the body's ability to fight off infections and heal injuries, including mouth sores. Other symptoms of zinc deficiency include hair loss, skin lesions, and diarrhea.
- Impaired Immune Response: Zinc is crucial for the development and function of immune cells. Deficiency leaves the body susceptible to infections that can cause mouth sores.
- Delayed Wound Healing: Zinc is essential for the production of collagen, a protein vital for tissue repair. Deficiency can slow down the healing process of mouth sores.
- Increased Susceptibility to Infections: A weakened immune system due to zinc deficiency makes the body more vulnerable to infections that can trigger or worsen mouth sores.
Riboflavin Deficiency and Mouth Sores
Riboflavin, also known as vitamin B2, is important for cell growth and energy production. A deficiency in riboflavin can cause inflammation of the mouth and throat, leading to mouth sores and a condition called angular cheilitis (cracks at the corners of the mouth). Other symptoms include skin rashes and eye problems.
- Inflammation of the Oral Mucosa: Riboflavin deficiency can directly lead to inflammation of the mucous membranes in the mouth, contributing to the formation of mouth sores.
- Impaired Cell Function: Riboflavin plays a critical role in energy production and cell function. Deficiency can impact cell repair and regeneration in the mouth.
- Angular Cheilitis: Riboflavin deficiency often manifests as angular cheilitis, cracks at the corners of the mouth, often accompanying mouth sores.
How do you get rid of mouth sores asap?

There's no single magic bullet for getting rid of mouth sores (canker sores or aphthous ulcers) instantly, as their healing time varies depending on size and severity. However, several methods can significantly speed up the healing process and alleviate discomfort. The key is to address the underlying cause (if known) and provide a soothing environment for the sore to heal. Over-the-counter remedies and good oral hygiene are crucial.
Over-the-Counter Remedies
Many effective over-the-counter treatments can ease the pain and promote faster healing. These often contain ingredients that numb the area (like benzocaine), reduce inflammation (like corticosteroids), or create a protective barrier. Always follow the package instructions carefully.
- Orajel or similar topical anesthetic: Provides temporary pain relief.
- Antiseptic mouthwashes: Can help prevent infection (e.g., chlorhexidine gluconate). However, be mindful that some mouthwashes can further irritate the sore.
- Creams or gels containing corticosteroids: These can reduce inflammation and accelerate healing. However, long-term use should be under the guidance of a dentist or doctor.
Home Remedies
Several home remedies can provide relief and potentially speed up healing. These are often gentler than some OTC options, but their effectiveness varies. It is important to maintain good oral hygiene while using these.
- Rinsing with salt water: A simple yet effective method to cleanse the area and reduce inflammation. Dissolve a teaspoon of salt in a glass of warm water and swish gently.
- Applying ice: Reduces swelling and numbs the area temporarily. Wrap an ice cube in a thin cloth before applying it directly to the sore.
- Using a baking soda paste: Create a paste with baking soda and water. Gently apply to the affected area, allowing it to sit for a few minutes before rinsing. It has antimicrobial and anti-inflammatory properties.
Dietary Changes
Certain foods and drinks can irritate mouth sores, prolonging healing time. Adjusting your diet can make a substantial difference.
- Avoid acidic foods and drinks: These can exacerbate pain and inflammation. This includes citrus fruits, tomatoes, and carbonated drinks.
- Limit spicy foods: Spicy foods can irritate the sore, increasing discomfort.
- Consume soft foods: Avoid foods that require excessive chewing, as this can cause further irritation to the sores. Opt for soft, easily digestible foods.
Maintaining Good Oral Hygiene
Proper oral hygiene is essential for preventing infection and promoting healing. Gentle brushing and flossing are crucial, but avoid directly scrubbing the sore.
- Brush gently: Use a soft-bristled toothbrush and brush gently around the affected area to avoid irritation.
- Floss carefully: Flossing is important for maintaining overall oral hygiene, but be extra gentle when flossing near the sore.
- Rinse regularly: Rinse your mouth with water or a prescribed mouthwash after eating and before bed.
When to See a Doctor
While most mouth sores heal on their own within a couple of weeks, it's vital to seek professional help if the sore persists for longer than three weeks, is excessively painful, is unusually large, bleeds frequently, or shows signs of infection (increased redness, swelling, or pus). Your dentist or doctor can determine the cause and recommend appropriate treatment.
- Persistent sores: Sores that don't heal within three weeks warrant a doctor's visit.
- Severe pain: Unbearable pain that interferes with eating or drinking should be addressed promptly.
- Signs of infection: Any signs of infection require immediate medical attention.
What is a viral illness that causes mouth sores?
The most common viral illness that causes mouth sores is herpes simplex virus (HSV), specifically HSV-1, although HSV-2 can also cause oral herpes. This virus is extremely common; most people are infected at some point in their lives, often during childhood. The infection can remain dormant in the nervous system and reactivate periodically, leading to outbreaks of cold sores or fever blisters. These sores typically appear on the lips, but can also occur inside the mouth. Other viruses, though less frequently, can also be responsible for mouth sores, but HSV is by far the most prevalent.
What are the Symptoms of Oral Herpes?
Oral herpes, or cold sores, typically begins with a tingling or burning sensation at the site of the upcoming lesion. This prodromal phase can last for several hours or even a day before the sores appear. The sores themselves start as small, fluid-filled blisters that eventually break open and form painful ulcers. These ulcers typically crust over and heal within 7-10 days. Some individuals may experience accompanying symptoms such as fever, headache, swollen lymph nodes, or general malaise.
- Tingling or burning sensation before lesion appearance.
- Fluid-filled blisters that break and form ulcers.
- Crusting and healing within 7-10 days.
How is Oral Herpes Transmitted?
Oral herpes is primarily transmitted through direct contact with an infected person, most commonly through kissing or sharing utensils, cups, or other items that come into contact with saliva. The virus can also be spread through touching an active lesion and then touching another part of the body or another person. It's important to note that the virus can be shed even when there are no visible sores, meaning transmission can occur even when someone is asymptomatic. Transmission from mother to child during birth is also possible.
- Direct contact with saliva (kissing).
- Sharing personal items (utensils, cups).
- Touching an active lesion and then touching another area or person.
What are the Treatment Options for Oral Herpes?
Unfortunately, there's no cure for oral herpes, but antiviral medications like acyclovir, valacyclovir, and famciclovir can help reduce the severity and duration of outbreaks. These medications are most effective when started at the first sign of an outbreak. Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help manage pain and discomfort. Topical anesthetics can also provide temporary relief from the pain of the sores. Keeping the sores clean and dry can also help promote healing.
- Antiviral medications (acyclovir, valacyclovir, famciclovir).
- Over-the-counter pain relievers (ibuprofen, acetaminophen).
- Topical anesthetics for pain relief.
Can I Prevent Oral Herpes Outbreaks?
While you can't completely prevent outbreaks if you've already been infected, you can take steps to reduce their frequency and severity. Avoiding triggers like stress, sunlight, and fever can be helpful. Maintaining good hygiene, such as washing your hands frequently, can also help prevent the spread of the virus. If you have an active outbreak, avoid kissing or sharing personal items to prevent transmission to others.
- Stress management.
- Sun protection.
- Good hygiene practices, including handwashing.
What is the most common cause of mouth sores?
The most common cause of mouth sores is a condition called aphthous stomatitis, often referred to as canker sores or mouth ulcers. These are small, shallow ulcers that typically appear on the inside of the lips, cheeks, or tongue. While the exact cause of canker sores remains unknown, several factors are believed to contribute to their development. Stress is a significant trigger for many individuals, as is minor trauma to the mouth, such as biting the cheek or accidentally scraping the gums. Nutritional deficiencies, particularly in iron, vitamin B12, or folic acid, can also increase the likelihood of developing canker sores. Certain food sensitivities, such as to acidic foods or ingredients like tomatoes or chocolate, have been linked to their occurrence in some people. Finally, hormonal changes, such as those experienced during menstruation, can also play a role in triggering canker sores in some women. It's important to note that while canker sores are usually not serious and resolve on their own within a week or two, recurring or persistent sores warrant a visit to a dentist or doctor to rule out any underlying medical conditions.
Can stress cause mouth sores?
Yes, stress is a well-documented trigger for mouth sores, particularly canker sores. While the exact mechanism isn't fully understood, it's believed that stress can weaken the immune system, making individuals more susceptible to developing these painful lesions. Chronic stress, in particular, seems to have a stronger correlation with the frequency and severity of canker sores. This is because ongoing stress can lead to a sustained inflammatory response in the body, which can manifest as mouth sores. Managing stress through techniques like yoga, meditation, or deep breathing exercises may help to reduce the frequency of mouth sore outbreaks. Furthermore, ensuring sufficient sleep and maintaining a healthy work-life balance are crucial aspects of stress management that can indirectly contribute to improved oral health and a reduction in the likelihood of developing mouth sores. If stress is a significant factor in your mouth sore occurrences, exploring stress reduction techniques and discussing potential coping mechanisms with a healthcare professional can be beneficial.
What other conditions can cause mouth sores?
While canker sores are the most frequent cause, various other conditions can lead to mouth sores. Herpes simplex virus (HSV), the virus responsible for cold sores, causes painful blisters that typically appear on the outer lip or surrounding skin. These are different from canker sores, which are found inside the mouth. Hand, foot, and mouth disease (HFMD), a common viral infection, can cause painful sores in the mouth alongside a rash on the hands and feet, mainly affecting children. Aphthous ulcers are another type of mouth sore, potentially caused by a range of factors such as trauma, stress, or immune system dysfunction. Oral thrush, a fungal infection caused by Candida albicans, can result in white patches and sores on the tongue and inner cheeks. Leukoplakia and oral lichen planus are less common but more serious conditions that can manifest as white or red patches and sores in the mouth; they may sometimes be precancerous. If you're experiencing unusual or persistent mouth sores, it is essential to seek professional medical advice to receive an accurate diagnosis and appropriate treatment.
When should I see a doctor about mouth sores?
Most canker sores heal within a week or two without treatment, but you should consult a doctor or dentist if you experience: persistent sores that don't heal after several weeks; recurrent sores that occur frequently; sores that are unusually large or painful; sores accompanied by fever, swollen lymph nodes, or other systemic symptoms; sores that appear different from previous sores; or if you have difficulty eating or drinking due to the sores. These symptoms could indicate an underlying medical condition requiring professional assessment and treatment. Similarly, if you have concerns about a possible infection or are experiencing sores that are interfering with your daily life, it's best to seek medical attention. A healthcare professional can accurately diagnose the cause of your mouth sores and recommend appropriate treatment or management strategies. Early intervention can be crucial in addressing more serious conditions, preventing complications, and ensuring optimal oral health.

Deja una respuesta