What is the sister disease to lupus
Lupus, a chronic autoimmune disease that can affect various organs and tissues, has a lesser-known companion disease that often goes unnoticed: Sjogren's syndrome. While both diseases share similarities in their autoimmune mechanisms and symptoms, there are distinct differences that set them apart. This article aims to shed light on the relationship between lupus and Sjogren's syndrome, exploring their shared characteristics, contrasting features, and the impact they have on affected individuals.
What is Considered a Sister Disease to Lupus?
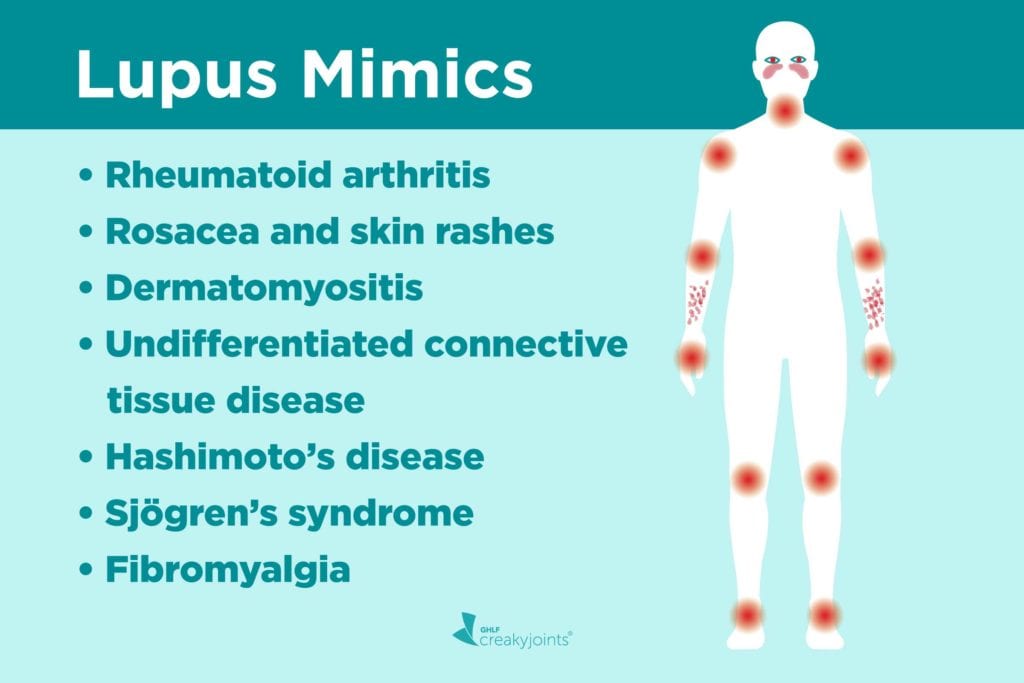
There isn't one single disease definitively labeled as lupus's "sister disease." However, several autoimmune diseases share similarities with lupus in terms of symptoms, pathogenesis, and genetic predisposition. These conditions often overlap or occur concurrently in the same individual, leading to the concept of a "sister disease" being used informally to describe this close relationship. The most commonly discussed candidates include Sjögren's syndrome, rheumatoid arthritis, and scleroderma, among others. The term "sister disease" is not a formal medical classification, but rather a helpful descriptive term for patients and their families to understand the potential interconnectedness of these conditions.
Sjögren's Syndrome as a Related Autoimmune Disease
Sjögren's syndrome is an autoimmune disease that primarily affects the moisture-producing glands, leading to dry eyes (keratoconjunctivitis sicca) and dry mouth (xerostomia). Many individuals with Sjögren's syndrome also have other autoimmune disorders, with lupus being a common comorbidity. The shared autoimmune mechanisms, overlapping symptoms, and frequent co-occurrence make Sjögren's a strong contender for the informal "sister disease" title. Genetic factors may play a role in the increased likelihood of both diseases occurring together.
Rheumatoid Arthritis and its Connection to Lupus
Rheumatoid arthritis (RA) is another autoimmune disease characterized by chronic inflammation of the joints. Similar to lupus, RA involves the immune system attacking the body's own tissues, resulting in pain, swelling, and stiffness. While the primary target tissues differ, there's significant overlap in genetic susceptibility and the presence of autoantibodies in both conditions. Furthermore, patients with lupus can develop RA, and vice versa, highlighting the potential for shared underlying mechanisms.
Scleroderma: Another Autoimmune Disease with Overlapping Features
Scleroderma is an autoimmune disease causing hardening and thickening of the skin and connective tissues. It shares some clinical features with lupus, particularly involving skin and organ involvement. Both conditions can cause inflammation, fatigue, and Raynaud's phenomenon (reduced blood flow to the extremities). Although distinct, the presence of overlapping autoantibodies and a similar autoimmune basis suggest a potential relationship, explaining why it's sometimes considered in the same category.
Overlap of Autoantibodies in Related Autoimmune Conditions
Several autoantibodies, proteins produced by the immune system that mistakenly attack the body's own tissues, are found in both lupus and related autoimmune conditions. For example, antinuclear antibodies (ANAs) are commonly present in lupus and other autoimmune diseases. The presence of similar autoantibodies further supports the idea of interconnected pathophysiological pathways.
Genetic Predisposition: Shared Risk Factors Across Autoimmune Diseases
Genetic factors play a crucial role in the development of both lupus and related autoimmune diseases. Studies have identified specific genes associated with an increased risk of developing lupus, and many of these same genes are also implicated in other autoimmune conditions. This shared genetic susceptibility provides further evidence for the close relationship between these diseases.
| Disease | Primary Target | Key Symptoms | Overlap with Lupus |
|---|---|---|---|
| Lupus | Connective tissue, multiple organs | Fatigue, joint pain, rash, fever, organ damage | High |
| Sjögren's Syndrome | Moisture-producing glands | Dry eyes, dry mouth, fatigue | Moderate to High |
| Rheumatoid Arthritis | Joints | Joint pain, swelling, stiffness | Moderate |
| Scleroderma | Skin, connective tissue | Skin thickening, Raynaud's phenomenon, organ damage | Moderate |
What is Considered a Sister Disease to Lupus?
There isn't one single disease definitively labeled as lupus's "sister disease." However, several autoimmune diseases share similarities with lupus in terms of symptoms, pathogenesis, and genetic predisposition. These conditions often overlap or occur concurrently in the same individual, leading to the concept of a "sister disease" being used informally to describe this close relationship. The most commonly discussed candidates include Sjögren's syndrome, rheumatoid arthritis, and scleroderma, among others. The term "sister disease" is not a formal medical classification, but rather a helpful descriptive term for patients and their families to understand the potential interconnectedness of these conditions.
Sjögren's Syndrome as a Related Autoimmune Disease
Sjögren's syndrome is an autoimmune disease that primarily affects the moisture-producing glands, leading to dry eyes (keratoconjunctivitis sicca) and dry mouth (xerostomia). Many individuals with Sjögren's syndrome also have other autoimmune disorders, with lupus being a common comorbidity. The shared autoimmune mechanisms, overlapping symptoms, and frequent co-occurrence make Sjögren's a strong contender for the informal "sister disease" title. Genetic factors may play a role in the increased likelihood of both diseases occurring together.
Rheumatoid Arthritis and its Connection to Lupus
Rheumatoid arthritis (RA) is another autoimmune disease characterized by chronic inflammation of the joints. Similar to lupus, RA involves the immune system attacking the body's own tissues, resulting in pain, swelling, and stiffness. While the primary target tissues differ, there's significant overlap in genetic susceptibility and the presence of autoantibodies in both conditions. Furthermore, patients with lupus can develop RA, and vice versa, highlighting the potential for shared underlying mechanisms.
Scleroderma: Another Autoimmune Disease with Overlapping Features
Scleroderma is an autoimmune disease causing hardening and thickening of the skin and connective tissues. It shares some clinical features with lupus, particularly involving skin and organ involvement. Both conditions can cause inflammation, fatigue, and Raynaud's phenomenon (reduced blood flow to the extremities). Although distinct, the presence of overlapping autoantibodies and a similar autoimmune basis suggest a potential relationship, explaining why it's sometimes considered in the same category.
Overlap of Autoantibodies in Related Autoimmune Conditions
Several autoantibodies, proteins produced by the immune system that mistakenly attack the body's own tissues, are found in both lupus and related autoimmune conditions. For example, antinuclear antibodies (ANAs) are commonly present in lupus and other autoimmune diseases. The presence of similar autoantibodies further supports the idea of interconnected pathophysiological pathways.
Genetic Predisposition: Shared Risk Factors Across Autoimmune Diseases
Genetic factors play a crucial role in the development of both lupus and related autoimmune diseases. Studies have identified specific genes associated with an increased risk of developing lupus, and many of these same genes are also implicated in other autoimmune conditions. This shared genetic susceptibility provides further evidence for the close relationship between these diseases.
| Disease | Primary Target | Key Symptoms | Overlap with Lupus |
|---|---|---|---|
| Lupus | Connective tissue, multiple organs | Fatigue, joint pain, rash, fever, organ damage | High |
| Sjögren's Syndrome | Moisture-producing glands | Dry eyes, dry mouth, fatigue | Moderate to High |
| Rheumatoid Arthritis | Joints | Joint pain, swelling, stiffness | Moderate |
| Scleroderma | Skin, connective tissue | Skin thickening, Raynaud's phenomenon, organ damage | Moderate |
What is worse, lupus or Sjögren's?
There is no single answer to the question of whether lupus or Sjögren's syndrome is "worse." Both are chronic autoimmune diseases that can cause significant disability and impact quality of life, but they affect different systems of the body and manifest with varying severity. The experience of each condition is highly individualized, meaning that the severity and impact vary greatly from person to person. What is more debilitating for one individual might be less severe for another, even with the same diagnosis. It's crucial to consider that the relative "worse" condition depends entirely on the individual's specific symptoms, the organs affected, and the overall impact on their daily life. Some individuals with lupus may experience mild symptoms manageable with medication, while others may face life-threatening complications. Similarly, Sjögren's syndrome can range from mild dryness to severe organ damage. Therefore, a direct comparison is not possible.
Severity and Range of Symptoms
Lupus is known for its wide-ranging symptoms that can affect numerous organ systems, including the skin, joints, kidneys, heart, lungs, and brain. This systemic nature contributes to its potential for severe complications. Lupus nephritis (kidney inflammation), for instance, is a potentially life-threatening complication. Sjögren's syndrome primarily affects the moisture-producing glands, leading to dryness of the eyes, mouth, and other mucous membranes. While it can cause significant discomfort and impact quality of life, its life-threatening complications are generally less frequent than those associated with lupus.
- Lupus: Can affect many organ systems leading to diverse and potentially severe symptoms.
- Sjögren's: Primarily affects moisture-producing glands, with symptoms mostly related to dryness.
- Severity Variation: Both diseases have a wide spectrum of severity, making direct comparison difficult.
Impact on Daily Life and Function
The impact on daily living depends heavily on the severity and specific symptoms experienced. For example, severe fatigue is a common symptom in both lupus and Sjögren's, which can significantly limit daily activities and productivity. The chronic pain associated with lupus arthritis can also have a profound impact on mobility and quality of life. Sjögren's dryness symptoms can cause challenges with eating, sleeping, and even vision, hindering daily tasks. Thus, the impact on daily life is highly individualized and not directly comparable between the two diseases.
- Fatigue: A common debilitating symptom in both conditions.
- Pain: Lupus often involves joint pain, impacting mobility significantly.
- Dryness: Sjögren's dryness can significantly impair daily functioning.
Treatment and Management
Both lupus and Sjögren's are managed with a variety of treatments aimed at controlling symptoms and preventing complications. Treatment approaches often involve medication, such as immunosuppressants, corticosteroids, and biologics. However, the specific treatments and their effectiveness vary depending on the individual's symptoms and disease activity. The lack of a cure for both conditions means that ongoing management is crucial. Both require careful monitoring and adjustments to treatment plans based on individual responses.
- Medications: Immunosuppressants, corticosteroids, and biologics are commonly used.
- Treatment Individualization: Treatment plans are tailored to each patient's needs.
- Long-Term Management: Both diseases require ongoing medical attention and treatment.
Potential Complications and Prognosis
Life-threatening complications are more frequently associated with lupus due to its systemic nature and potential to affect vital organs. Kidney failure, cardiovascular disease, and central nervous system involvement are significant concerns in lupus. Sjögren's syndrome, while causing considerable discomfort and impacting quality of life, is less likely to result in directly life-threatening complications, although it can lead to secondary infections or other problems due to compromised immunity and dryness.
- Lupus Complications: Kidney failure, cardiovascular issues, central nervous system complications are serious risks.
- Sjögren's Complications: Increased risk of infections and other issues related to dryness and compromised immunity.
- Prognosis: Both conditions have varied prognoses depending on individual symptoms, treatment response and other factors.
Overall Quality of Life
Ultimately, determining which condition is "worse" is subjective and depends on individual experiences. Quality of life is impacted differently in each case, with some individuals experiencing more significant limitations than others, regardless of the specific diagnosis. Factors like symptom severity, treatment response, support systems, and overall emotional well-being play critical roles in determining overall quality of life for both conditions.
- Individual Variation: The impact on quality of life varies greatly depending on individual factors.
- Symptom Severity: The intensity and frequency of symptoms influence quality of life.
- Emotional Well-being: Mental health plays a crucial role in adapting to and coping with chronic illness.
What is the deadliest autoimmune disease?
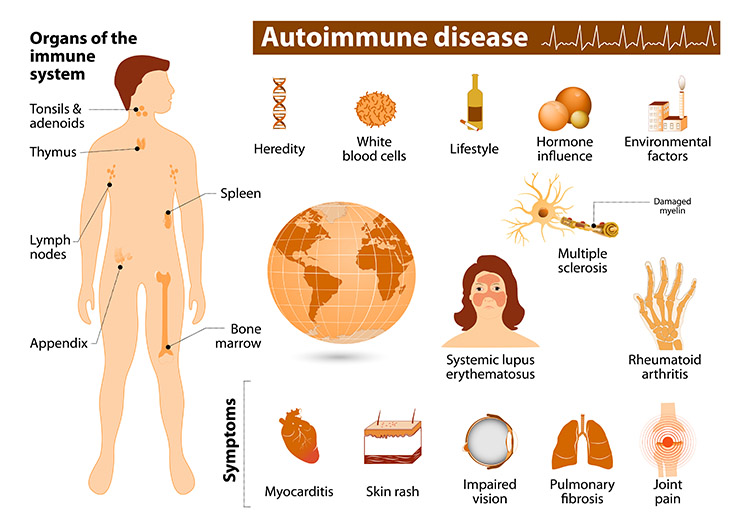
There is no single "deadliest" autoimmune disease. Mortality rates vary significantly depending on the specific disease, its severity, the individual's overall health, access to treatment, and timely diagnosis. Many autoimmune diseases can be life-threatening if left untreated, leading to organ failure or other severe complications. The impact of a particular disease also depends on factors like the age of onset and the presence of comorbidities.
What are some of the most serious autoimmune diseases?
Several autoimmune diseases carry a significant risk of mortality if not properly managed. These include systemic lupus erythematosus (SLE), rheumatoid arthritis (RA) with severe complications, and multiple sclerosis (MS) with progressive disability. However, even within these diseases, the risk of death varies dramatically depending on individual factors. Early diagnosis and effective treatment strategies are crucial in mitigating the severity and improving the prognosis for all autoimmune diseases.
- Systemic lupus erythematosus (SLE) can affect multiple organ systems, leading to severe complications.
- Rheumatoid arthritis (RA), if left untreated, can cause debilitating joint damage and increase the risk of cardiovascular issues.
- Multiple sclerosis (MS) can lead to progressive neurological disability, impacting various bodily functions.
How does treatment affect mortality rates?
Access to effective and timely treatment significantly impacts mortality rates associated with autoimmune diseases. Advances in medical understanding and treatment options have dramatically improved outcomes for many individuals. Early diagnosis is crucial, allowing for prompt initiation of treatment, which can prevent or delay disease progression and reduce the risk of serious complications. Treatment strategies vary depending on the specific disease and the individual's condition, often including immunosuppressants, biologics, or other targeted therapies.
- Improved medications have decreased mortality rates in many autoimmune diseases.
- Access to specialists and advanced treatments is vital for better outcomes.
- Early intervention and proactive management are key in preventing severe complications.
What are the leading causes of death in autoimmune diseases?
The leading causes of death in individuals with autoimmune diseases are often related to complications arising from the disease itself. These can include organ failure (kidney, heart, lung), infections due to immunosuppressive therapies, and cardiovascular events. The underlying autoimmune process frequently contributes to these complications, making the management of the disease a crucial factor in preventing mortality. Other contributing factors can include the individual's age, presence of comorbidities, and overall health status.
- Organ failure is a significant cause of death in severe cases.
- Infections can be life-threatening due to immunosuppressive treatments.
- Cardiovascular diseases are a common cause of mortality in many autoimmune patients.
How are autoimmune diseases diagnosed and monitored?
Diagnosis of autoimmune diseases often involves a combination of physical examinations, blood tests (to detect autoantibodies), imaging studies (such as MRI or CT scans), and possibly biopsies. Monitoring usually involves regular check-ups with specialists, periodic blood tests to track disease activity, and assessments of organ function. Regular monitoring and adherence to the treatment plan are crucial for managing the disease effectively and preventing severe complications. This allows for timely adjustments to the treatment plan as needed.
- Blood tests are used to detect the presence of autoantibodies.
- Imaging studies help assess organ damage and disease progression.
- Regular monitoring is key for early detection of complications.
What is the role of research in improving outcomes?
Ongoing research plays a vital role in understanding the underlying causes of autoimmune diseases, developing more effective treatments, and ultimately improving patient outcomes. Research efforts focus on identifying new therapeutic targets, developing safer and more effective drugs, and improving diagnostic techniques. Investing in research is crucial for advancing the treatment and management of autoimmune diseases and reducing their mortality rates.
- Research is focused on identifying new therapeutic targets.
- Development of new and improved treatments is ongoing.
- Research leads to better diagnostic tools and improved management strategies.
What were your first symptoms of Sjögren's?
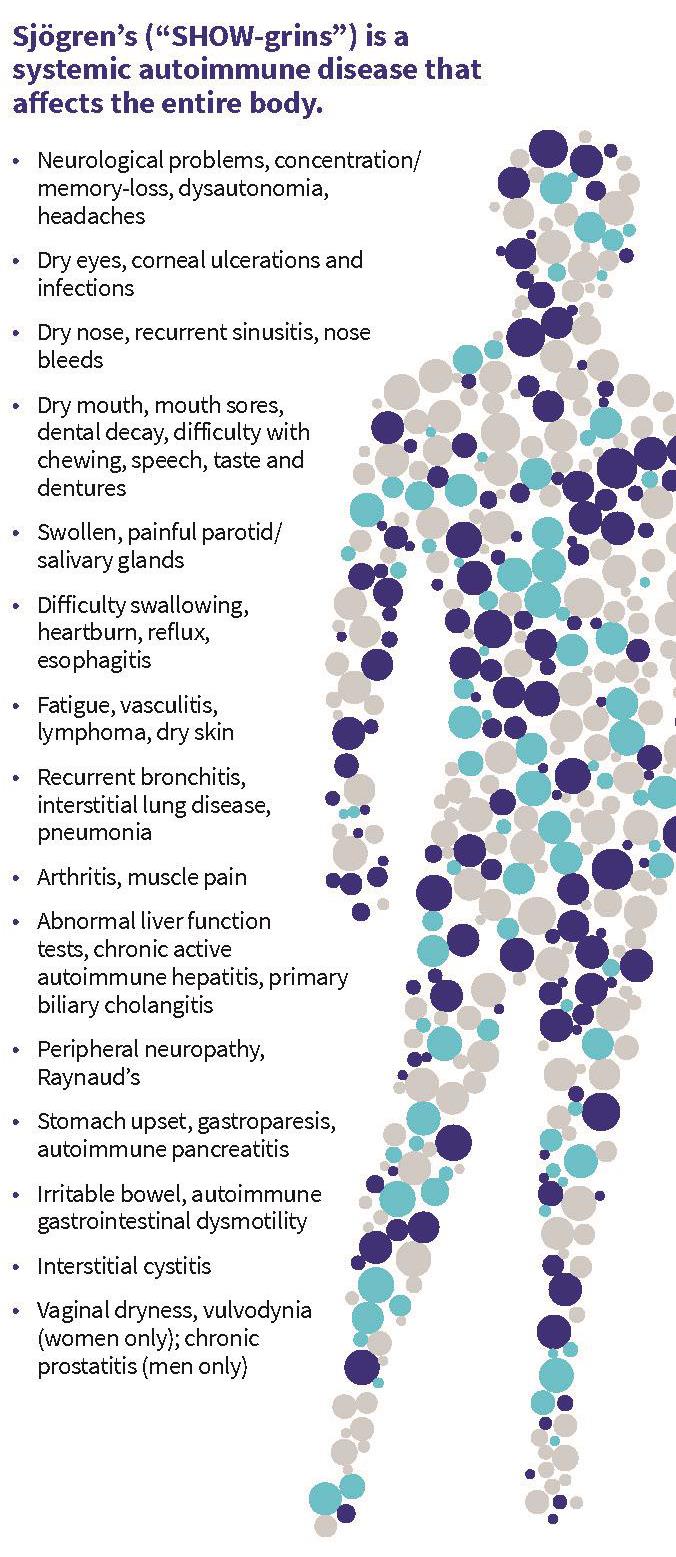
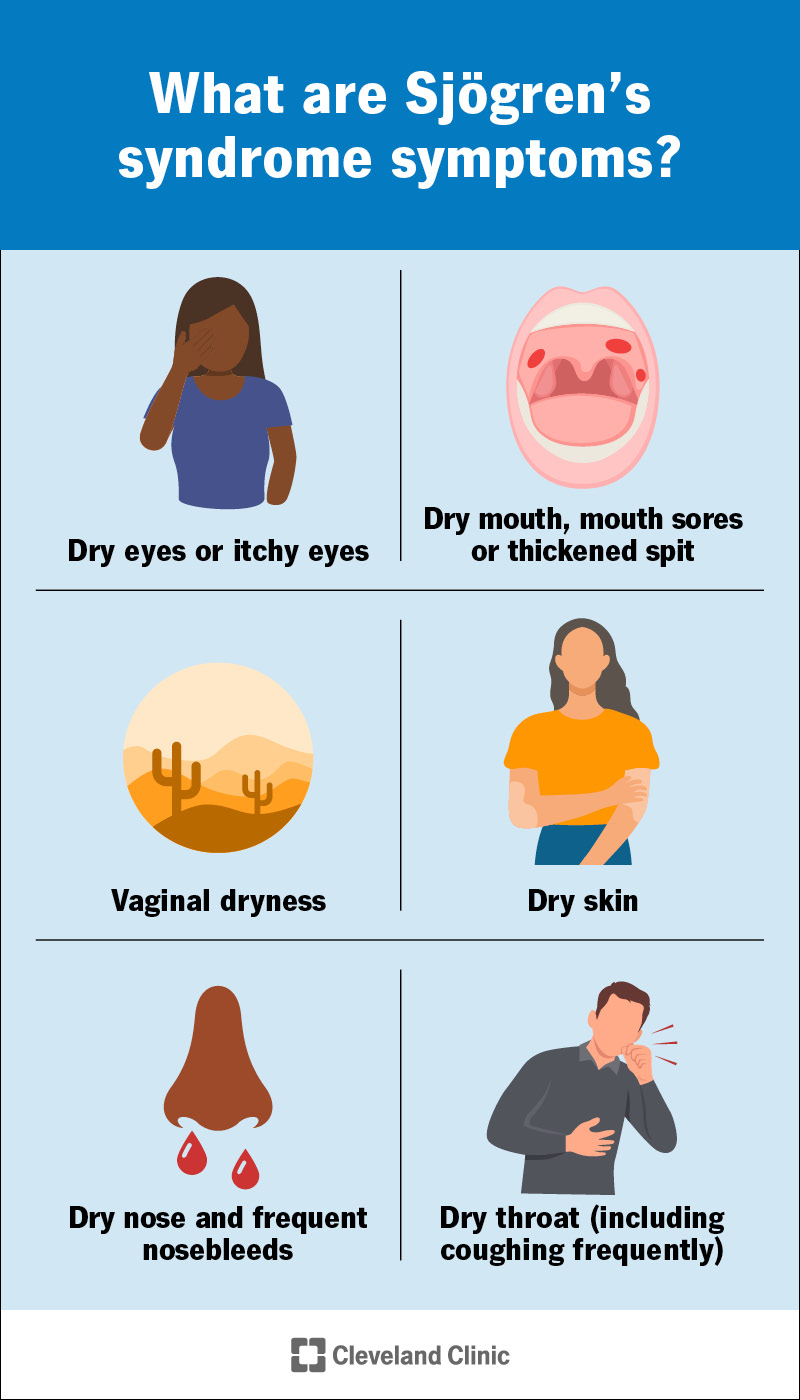
As a large language model, I don't have a body and therefore cannot experience medical conditions like Sjögren's syndrome. I can, however, provide information based on commonly reported early symptoms. The initial symptoms are often subtle and can be easily attributed to other conditions, making diagnosis challenging. They typically involve dryness of the eyes and mouth, but can also include other symptoms like fatigue and joint pain. The severity and combination of symptoms vary widely between individuals.
Dry Eyes
Dry eyes are a very common early sign of Sjögren's. This dryness isn't just a feeling of occasional dryness; it's a persistent, often uncomfortable, sensation. It can lead to a burning, gritty feeling, excessive tearing (ironically, the body's attempt to compensate for dryness), and blurry vision. The dryness is caused by a lack of sufficient lubrication in the eyes due to the autoimmune attack on the tear glands. This can lead to significant discomfort and even damage to the cornea if left untreated.
- Burning and stinging sensation in the eyes
- Excessive tearing (paradoxical dryness)
- Blurred vision, especially in low light
Dry Mouth
Dry mouth (xerostomia) is another hallmark symptom. This isn't simply feeling a little thirsty; it's a persistent dryness that can make it difficult to swallow, speak, or even taste food properly. It's caused by the autoimmune destruction of the salivary glands, reducing saliva production significantly. This can also increase the risk of dental problems like cavities and gum disease.
- Difficulty swallowing, especially dry foods
- Persistent thirst, even after drinking fluids
- Changes in taste or a metallic taste in the mouth
Fatigue
Fatigue, a feeling of overwhelming tiredness and exhaustion, is often one of the first noticeable symptoms for many individuals with Sjögren's. It is not the kind of tiredness that can be relieved by a good night's sleep, but rather a persistent, debilitating tiredness that impacts daily activities. This fatigue is not solely explained by dry eyes and mouth but is believed to be linked to the underlying autoimmune process and its systemic effects on the body.
- Persistent tiredness and lack of energy
- Difficulty concentrating and focusing
- Reduced physical stamina, even for simple tasks
Joint Pain (Arthralgia)
Many individuals experience joint pain and stiffness (arthralgia) as one of their first symptoms of Sjögren's. This pain is often described as achy, migratory pain, meaning that it may move from one joint to another. It may not be as severe or debilitating as the joint pain seen in rheumatoid arthritis, but it can significantly impact daily activities and quality of life. This is because the autoimmune response can also affect the joints.
- Aching and stiffness in joints
- Pain that migrates between different joints
- Swelling and tenderness around affected joints (less common than in rheumatoid arthritis)
Other Symptoms
Besides the primary symptoms, several other less common, but still significant symptoms, can appear early on. These can include a persistent dry cough, vaginal dryness, skin dryness, and frequent urinary tract infections. The presence of these symptoms along with the more common initial symptoms often points to a broader picture of Sjögren's Syndrome and should prompt further medical investigation. It is crucial to note that these symptoms can also be associated with other conditions and need to be properly evaluated by medical professionals.
- Dry cough
- Vaginal dryness
- Skin dryness and rashes
- Frequent urinary tract infections
What is the life expectancy of someone with lupus in the brain?
:max_bytes(150000):strip_icc()/VWHNewCreate-Lupus-e80d89d3b3ff4b38b798f9e84468f04c.png)
There isn't a single, definitive answer to the question of life expectancy for someone with neuropsychiatric lupus (NPSLE), also known as lupus in the brain. This is because the severity and specific manifestations of NPSLE vary greatly from person to person. The impact on life expectancy depends on several factors, including the specific neurological symptoms, the presence of other organ involvement (such as kidney or heart disease), the individual's overall health, and the effectiveness of treatment. While NPSLE can significantly impact quality of life and may lead to disability, it doesn't automatically drastically shorten lifespan for all individuals. Some individuals with mild NPSLE may experience only minor symptoms and have a normal life expectancy, while others with severe and widespread neurological involvement may face more significant health challenges impacting their lifespan. Accurate prediction of life expectancy is difficult and dependent on a case-by-case assessment by medical professionals.
Factors Affecting Life Expectancy in NPSLE
Several factors contribute to the variability in life expectancy among individuals with NPSLE. These factors need to be considered individually for each patient. Early diagnosis and aggressive treatment can significantly improve outcomes. However, the unpredictable nature of the disease makes long-term prognosis challenging.
- Severity of Neurological Symptoms: The more severe and widespread the neurological symptoms, the greater the potential impact on life expectancy.
- Presence of Other Organ Involvement: Lupus is a systemic disease, meaning it can affect multiple organs. The presence of kidney disease (lupus nephritis), heart problems (lupus carditis), or lung involvement can significantly affect overall health and survival.
- Treatment Response: The effectiveness of treatments in managing symptoms and preventing complications plays a crucial role in influencing life expectancy.
The Role of Early Diagnosis and Treatment
Early diagnosis and prompt initiation of appropriate treatment are critical in managing NPSLE and improving outcomes. Early intervention can help prevent or minimize the severity of neurological complications. Regular monitoring and adjustments to treatment plans as needed are essential for long-term management.
- Immunosuppressant medications: These drugs help reduce the inflammation and immune system activity that causes lupus.
- Corticosteroids: These powerful anti-inflammatory medications can effectively reduce symptoms, but long-term use has side effects.
- Other treatments: Depending on the specific symptoms, other therapies like physical therapy, occupational therapy, and cognitive behavioral therapy may be helpful.
Comorbidities and Their Impact
Individuals with NPSLE often have other health conditions (comorbidities) that can further complicate their prognosis and affect life expectancy. Managing these comorbidities effectively is crucial. These comorbidities can be directly or indirectly related to lupus.
- Cardiovascular disease: Lupus increases the risk of heart disease and stroke.
- Kidney disease: Lupus nephritis can lead to kidney failure, requiring dialysis or transplantation.
- Infections: Immunosuppressant medications can increase susceptibility to infections.
Challenges in Assessing Life Expectancy
Predicting life expectancy for individuals with NPSLE is complex due to the disease's heterogeneous nature and unpredictable course. Each person’s experience is unique, making generalizations unreliable.
- Variability in Disease Presentation: NPSLE can manifest in a wide range of neurological symptoms.
- Individual Response to Treatment: Responses to medications and therapies vary greatly.
- Lack of Large-Scale Longitudinal Studies: More research is needed to accurately define the long-term prognosis of NPSLE.
Importance of Multidisciplinary Care
Optimal management of NPSLE requires a multidisciplinary approach involving rheumatologists, neurologists, nephrologists (if kidney involvement is present), and other specialists as needed. This collaborative care model ensures comprehensive assessment and treatment of the various aspects of the disease and associated complications. Regular monitoring of both lupus activity and organ damage is crucial for long-term health management.
- Rheumatologist: Manages the overall lupus condition.
- Neurologist: Focuses on the neurological manifestations.
- Other specialists: Cardiologist, nephrologist, pulmonologist, etc., as needed.
What is considered a sister disease to lupus?
There isn't one single disease definitively labeled as the "sister disease" to lupus. Lupus is a complex autoimmune disease with diverse manifestations, making it difficult to pinpoint a single counterpart. However, several autoimmune conditions share similarities with lupus in terms of their underlying mechanisms, symptoms, and affected populations. These conditions frequently overlap or co-occur with lupus, making them clinically relevant comparisons. Sjögren's syndrome, for instance, is often associated with lupus, with many patients experiencing both conditions. Both involve the immune system attacking moisture-producing glands, leading to dry eyes and mouth. Similarly, rheumatoid arthritis, while affecting primarily the joints, shares autoimmune origins with lupus and may manifest alongside it. The presence of shared autoantibodies and overlapping symptoms makes understanding these connections crucial for diagnosis and treatment. Furthermore, scleroderma, characterized by hardening and thickening of the skin, and mixed connective tissue disease (MCTD), exhibiting features of several connective tissue diseases including lupus, share genetic predispositions and overlapping clinical presentations with lupus. These conditions are often considered related, not necessarily as "sister diseases" but as members of the same autoimmune disease family. It's important to note that the term "sister disease" isn't a formally recognized medical classification, rather it's a colloquial comparison highlighting the similarities and potential co-occurrence of these conditions. The exact relationship and clinical implications vary significantly between individuals.
Are there other autoimmune diseases closely related to lupus?
Yes, several other autoimmune diseases share significant similarities with lupus. The overlapping features often make accurate diagnosis challenging, requiring extensive testing and clinical observation. As mentioned before, Sjögren's syndrome, rheumatoid arthritis, and scleroderma frequently co-occur with lupus or present with similar symptoms. Beyond these, other autoimmune diseases exhibit connections through shared genetic factors or similar immune system dysfunction. Systemic sclerosis, like scleroderma, involves the thickening and hardening of the skin and internal organs. Polymyositis/dermatomyositis, which involves muscle inflammation, also has some overlapping characteristics. The connection stems from the shared underlying mechanism – an overactive immune system attacking the body's own tissues. The exact nature and extent of these relationships are still under investigation, but the understanding of these overlaps is crucial for improving diagnostic strategies and treatment approaches. Research continues to unravel the intricate network of autoimmune disorders, revealing more about their interrelationships and informing better patient care.
How similar are the symptoms of lupus and its "sister diseases"?
The symptom overlap between lupus and related autoimmune conditions can be substantial, adding complexity to diagnosis. While each disease has distinct characteristics, several symptoms are common across these conditions. Fatigue, for example, is a prominent symptom of lupus and often appears in Sjögren's syndrome, rheumatoid arthritis, and other autoimmune disorders. Joint pain and inflammation (arthritis) are frequently seen in lupus, rheumatoid arthritis, and other connective tissue diseases. Similarly, skin rashes, though varying in presentation, can occur in lupus, scleroderma, and dermatomyositis. Kidney problems are a significant complication of lupus, but kidney involvement can also occur in other autoimmune diseases, though less frequently. However, it's important to remember that the severity and specific manifestation of these symptoms vary considerably between individuals and among diseases. The presence of certain symptoms, such as the characteristic butterfly rash in lupus, might help clinicians differentiate between these conditions. Nonetheless, diagnostic testing, including blood tests for specific autoantibodies, is essential for accurate identification and tailored treatment planning. The complexity of these overlapping symptoms underscores the need for a thorough medical evaluation involving specialists familiar with autoimmune disorders.
Does having one autoimmune disease increase the risk of developing lupus?
Having one autoimmune disease significantly increases the risk of developing another, including lupus. This increased susceptibility stems from the shared genetic and environmental factors influencing the development of these disorders. Individuals with a family history of autoimmune conditions, including lupus, have a heightened risk of developing multiple autoimmune diseases. The underlying immune system dysregulation, which is central to these disorders, likely plays a crucial role. If the immune system is already prone to attacking the body's own tissues in one area, it's more likely to do so in others. This means that someone diagnosed with rheumatoid arthritis, for example, has a statistically higher chance of subsequently developing lupus compared to the general population. Similarly, those with Sjögren's syndrome, scleroderma, or other connective tissue diseases are at increased risk. This highlights the importance of regular check-ups and vigilant monitoring for any new symptoms, particularly in individuals with a pre-existing autoimmune disease. Early detection and proactive management of autoimmune conditions can often improve outcomes and prevent serious complications. Further research is needed to completely elucidate the mechanisms behind this increased risk and develop strategies for prevention.
Deja una respuesta