Why do I suddenly have sores all over my mouth

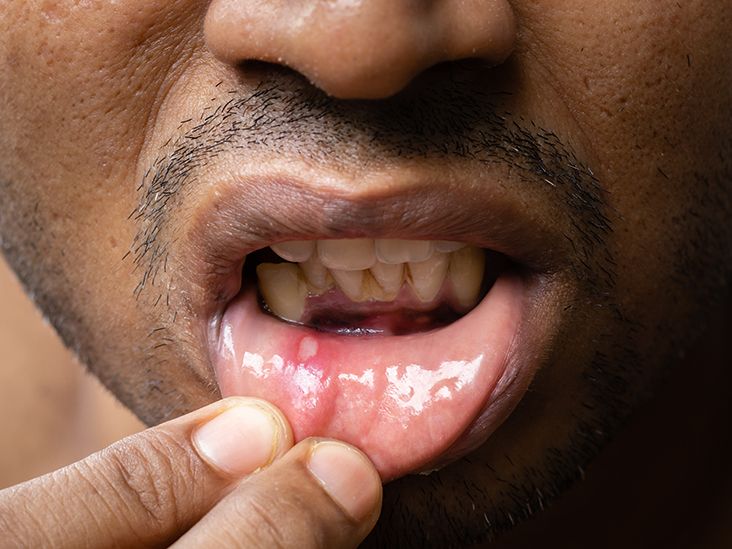
Do you wake up one morning with a burning sensation in your mouth, accompanied by painful sores? These sores, medically known as stomatitis, can make eating, drinking, and talking uncomfortable. While stomatitis can stem from various causes, understanding its origins is crucial to finding effective treatment. In this article, we delve into the potential reasons behind the sudden appearance of mouth sores, exploring the role of underlying health conditions, dietary factors, and lifestyle habits. By shedding light on these possible causes, we aim to equip you with the knowledge necessary to manage and prevent future outbreaks of mouth sores.
Why Do I Suddenly Have Sores All Over My Mouth?
Sudden onset of multiple mouth sores can be alarming and indicate a variety of underlying issues. It's crucial to understand that I cannot provide medical advice, and self-diagnosing can be dangerous. This information is for educational purposes only, and you should always consult a doctor or dentist for a proper diagnosis and treatment plan if you're experiencing this symptom.
Viral Infections
Many viral infections, like the common cold or the flu, can manifest as mouth sores. These sores are often small, painful blisters or ulcers that can appear anywhere in the mouth. Herpes simplex virus (HSV), the virus responsible for cold sores, is a particularly common cause. Other viral infections like hand, foot, and mouth disease can also present with mouth sores, especially in children. The sores usually resolve on their own within a week or two, but symptomatic treatment like pain relievers can help manage discomfort.
Bacterial Infections
While less common than viral infections, bacterial infections can also cause mouth sores. Streptococcal infections, for example, can lead to painful ulcers. Poor oral hygiene or weakened immune systems can increase the risk of bacterial infections in the mouth. Treatment typically involves antibiotics prescribed by a doctor. It's important to maintain good oral hygiene to prevent further complications.
Stress
Believe it or not, stress can significantly impact your oral health. When you're under a lot of stress, your immune system can be weakened, making you more susceptible to infections and potentially leading to mouth sores. Chronic stress can also exacerbate existing oral health problems. Managing stress through techniques like exercise, meditation, or yoga may help reduce the frequency and severity of mouth sores.
Nutritional Deficiencies
Certain nutritional deficiencies, particularly deficiencies in vitamin B12, iron, and folic acid, can contribute to mouth sores. These vitamins are essential for maintaining healthy mucous membranes in the mouth. A balanced diet rich in fruits, vegetables, and whole grains can help prevent nutritional deficiencies. If you suspect a deficiency, a blood test can confirm the diagnosis, and supplementation may be necessary.
Allergies and Reactions
Mouth sores can also be a reaction to certain foods, medications, or dental products. An allergic reaction to toothpaste, mouthwash, or even certain foods can manifest as sores or irritation in the mouth. Identifying and avoiding the allergen is crucial. If you suspect an allergic reaction, consult an allergist for testing and advice.
| Possible Cause | Symptoms | Treatment |
|---|---|---|
| Viral Infections (HSV, common cold) | Small, painful blisters or ulcers; fever (sometimes) | Pain relievers; antiviral medication (for HSV) |
| Bacterial Infections (Streptococcal) | Painful ulcers; possible fever; swelling | Antibiotics |
| Stress | Variety of sores; often linked to other stress symptoms | Stress management techniques; possibly supportive oral care |
| Nutritional Deficiencies (B12, Iron, Folic Acid) | Soreness; pale gums; fatigue (often other symptoms) | Dietary changes; supplements (as prescribed by a doctor) |
| Allergies/Reactions | Itching, burning, swelling; possibly localized to area of contact | Identify and avoid allergen; antihistamines (if needed) |
Why Do I Suddenly Have Sores All Over My Mouth?
Sudden onset of multiple mouth sores can be alarming and indicate a variety of underlying issues. It's crucial to understand that I cannot provide medical advice, and self-diagnosing can be dangerous. This information is for educational purposes only, and you should always consult a doctor or dentist for a proper diagnosis and treatment plan if you're experiencing this symptom.
Viral Infections
Many viral infections, like the common cold or the flu, can manifest as mouth sores. These sores are often small, painful blisters or ulcers that can appear anywhere in the mouth. Herpes simplex virus (HSV), the virus responsible for cold sores, is a particularly common cause. Other viral infections like hand, foot, and mouth disease can also present with mouth sores, especially in children. The sores usually resolve on their own within a week or two, but symptomatic treatment like pain relievers can help manage discomfort.
Bacterial Infections
While less common than viral infections, bacterial infections can also cause mouth sores. Streptococcal infections, for example, can lead to painful ulcers. Poor oral hygiene or weakened immune systems can increase the risk of bacterial infections in the mouth. Treatment typically involves antibiotics prescribed by a doctor. It's important to maintain good oral hygiene to prevent further complications.
Stress
Believe it or not, stress can significantly impact your oral health. When you're under a lot of stress, your immune system can be weakened, making you more susceptible to infections and potentially leading to mouth sores. Chronic stress can also exacerbate existing oral health problems. Managing stress through techniques like exercise, meditation, or yoga may help reduce the frequency and severity of mouth sores.
Nutritional Deficiencies
Certain nutritional deficiencies, particularly deficiencies in vitamin B12, iron, and folic acid, can contribute to mouth sores. These vitamins are essential for maintaining healthy mucous membranes in the mouth. A balanced diet rich in fruits, vegetables, and whole grains can help prevent nutritional deficiencies. If you suspect a deficiency, a blood test can confirm the diagnosis, and supplementation may be necessary.
Allergies and Reactions
Mouth sores can also be a reaction to certain foods, medications, or dental products. An allergic reaction to toothpaste, mouthwash, or even certain foods can manifest as sores or irritation in the mouth. Identifying and avoiding the allergen is crucial. If you suspect an allergic reaction, consult an allergist for testing and advice.
| Possible Cause | Symptoms | Treatment |
|---|---|---|
| Viral Infections (HSV, common cold) | Small, painful blisters or ulcers; fever (sometimes) | Pain relievers; antiviral medication (for HSV) |
| Bacterial Infections (Streptococcal) | Painful ulcers; possible fever; swelling | Antibiotics |
| Stress | Variety of sores; often linked to other stress symptoms | Stress management techniques; possibly supportive oral care |
| Nutritional Deficiencies (B12, Iron, Folic Acid) | Soreness; pale gums; fatigue (often other symptoms) | Dietary changes; supplements (as prescribed by a doctor) |
| Allergies/Reactions | Itching, burning, swelling; possibly localized to area of contact | Identify and avoid allergen; antihistamines (if needed) |
Why do I have a bunch of sores in my mouth all of a sudden?

The sudden appearance of multiple sores in your mouth could be due to several reasons, and it's impossible to diagnose the specific cause without a medical examination. However, some common culprits include:
Viral infections: Herpes simplex virus (HSV) is a frequent cause of oral herpes, characterized by cold sores or fever blisters. Other viral infections can also manifest as mouth sores. The sores may be painful, blister-like, and may cluster together.
Bacterial infections: Although less common than viral infections, bacterial infections can cause mouth sores. These might appear as ulcers or inflamed areas. Poor oral hygiene can increase the risk of bacterial infections.
Fungal infections: Oral thrush, caused by the Candidafungus, is another possibility. This often presents as creamy white lesions on the tongue, inner cheeks, or roof of the mouth. It's more common in individuals with weakened immune systems.
Traumatic injury: Accidental biting of the cheek or tongue, ill-fitting dentures, or even aggressive brushing can cause sores. These are usually localized and may heal relatively quickly.
Nutritional deficiencies: Deficiencies in certain vitamins and minerals, like B vitamins and iron, can sometimes contribute to mouth sores.
Allergies: Certain foods or oral hygiene products can trigger allergic reactions manifesting as mouth sores. This reaction may include swelling, itching, or painful lesions.
Autoimmune diseases: Certain autoimmune diseases can cause mouth sores as a symptom. These diseases involve the body's immune system attacking its own tissues.
It's crucial to consult a doctor or dentist for a proper diagnosis and treatment plan. Self-treating can be risky and may delay appropriate care.
Possible Causes of Sudden Mouth Sores
The sudden onset of multiple mouth sores is a common problem with various potential underlying causes. Viral infections like herpes simplex are a leading cause, presenting as painful blisters. Bacterial infections, often linked to poor oral hygiene, can also contribute. Fungal infections, such as oral thrush, frequently appear as creamy white patches. Less common causes include physical trauma from biting or ill-fitting dentures, nutritional deficiencies, allergic reactions to food or oral products, and underlying autoimmune diseases.
- Viral infections: Herpes simplex virus (HSV) is a primary culprit, causing cold sores or fever blisters. Other viral infections can also result in mouth sores.
- Bacterial infections: Poor oral hygiene can increase the risk of bacterial infections leading to mouth sores. These infections often manifest as ulcers or inflammation.
- Fungal infections: Oral thrush, caused by Candida albicans, is a common fungal infection characterized by creamy white patches.
Identifying the Type of Mouth Sore
Different types of mouth sores have distinct characteristics that can help in diagnosis. Cold sores usually appear as clustered blisters, while canker sores are typically small, shallow ulcers. Oral thrush presents as creamy white patches, often accompanied by a burning sensation. Traumatic ulcers are usually localized to the site of injury. Carefully observing the appearance, location, and symptoms of your sores can assist a healthcare professional in determining the underlying cause.
- Appearance: Note the color, size, shape, and texture of the sores.
- Location: The location of the sores can provide clues. For example, cold sores often appear on the lips or around the mouth.
- Symptoms: Pay attention to accompanying symptoms such as pain, burning, swelling, or fever.
When to Seek Medical Attention
While many mouth sores resolve on their own, certain situations warrant immediate medical attention. Severe pain, high fever, difficulty swallowing or breathing, or sores that don't heal within two weeks all require prompt evaluation by a doctor or dentist. Furthermore, if you have a weakened immune system, any new mouth sores should be checked by a healthcare professional to rule out serious infections.
- Persistent sores: Sores that don't heal within two weeks require medical attention.
- Severe symptoms: High fever, difficulty swallowing, or severe pain are warning signs.
- Weakened immune system: Individuals with compromised immune systems should seek medical attention for any mouth sores.
Home Remedies and Over-the-Counter Treatments
For mild mouth sores, some home remedies may provide temporary relief. Rinsing your mouth with warm salt water can help to clean the area and reduce inflammation. Applying a cold compress can soothe pain. Over-the-counter pain relievers like ibuprofen or acetaminophen can help manage discomfort. However, it's crucial to remember that these remedies are for symptom relief and not a cure, and should not replace a visit to the doctor or dentist for proper diagnosis and treatment.
- Salt water rinse: Dissolve ½ to ¾ teaspoon of salt in 8 ounces of warm water and rinse several times a day.
- Cold compress: Apply a cold compress to the affected area for 10-15 minutes at a time.
- Over-the-counter pain relievers: Use as directed to reduce pain and inflammation.
Importance of Maintaining Good Oral Hygiene
Good oral hygiene plays a vital role in preventing and managing mouth sores. Brushing your teeth twice daily with fluoride toothpaste, flossing regularly, and using a mouthwash can help to reduce the risk of infection. Regular dental check-ups are also important for early detection and treatment of any oral health issues. Avoid irritants such as acidic foods and beverages which may exacerbate existing sores.
- Brushing and flossing: Maintain a consistent routine of brushing and flossing to remove food particles and plaque.
- Mouthwash: Use an alcohol-free mouthwash to help soothe and clean the mouth.
- Regular dental checkups: Schedule regular checkups to address any potential issues early.
What causes a sore all over the mouth?
What Causes a Sore All Over the Mouth?
A sore all over the mouth, meaning widespread mouth pain and discomfort, can have several underlying causes. It's crucial to understand that this isn't a specific diagnosis but a symptom pointing to various potential problems. The severity, location, and accompanying symptoms will help determine the underlying cause. A widespread sore mouth often indicates a more systemic issue rather than a localized infection. Seeking professional medical advice is always recommended to get an accurate diagnosis and appropriate treatment.
Viral Infections
Viral infections, particularly those affecting the mucous membranes of the mouth, are common culprits. These infections often present with widespread sores, pain, and inflammation. The herpes simplex virus (HSV), responsible for oral herpes (cold sores), can sometimes cause widespread outbreaks, especially in individuals with weakened immune systems. Other viruses can also contribute to generalized mouth sores.
- Herpes simplex virus (HSV): Causes cold sores, sometimes widespread.
- Hand, foot, and mouth disease: A viral infection causing sores in the mouth and on hands and feet.
- Other viral infections: Various other viruses can contribute to mouth sores as a symptom.
Bacterial Infections
Although less common than viral causes for widespread mouth sores, bacterial infections can also be responsible. These infections often involve a secondary infection, meaning a bacterial infection complicates an existing condition like a viral infection or injury. Poor oral hygiene can significantly increase the risk of bacterial infections leading to mouth sores.
- Streptococcal infections: Can lead to severe mouth inflammation and sores.
- Secondary infections: Bacteria can infect an existing mouth injury or viral infection.
- Poor oral hygiene: Creates a breeding ground for harmful bacteria.
Fungal Infections
Fungal infections, most notably oral thrush (candidiasis), can cause widespread mouth sores and discomfort. Oral thrush is caused by an overgrowth of the Candida fungus, often occurring in individuals with weakened immune systems, those taking certain medications (like antibiotics), or those with poorly controlled diabetes. The sores typically appear as white patches or lesions.
- Oral thrush (candidiasis): Caused by Candida fungus overgrowth.
- Weakened immune system: Increases susceptibility to fungal infections.
- Medication side effects: Some medications can disrupt the oral flora, increasing the risk of thrush.
Allergic Reactions
Allergic reactions to foods, medications, or other substances can manifest as widespread mouth sores. These reactions can range from mild irritation and inflammation to severe reactions involving significant swelling and discomfort. Identifying the allergen is crucial for managing this type of mouth sore.
- Food allergies: Reactions to certain foods can cause mouth irritation and sores.
- Medication allergies: Some medications can trigger allergic reactions affecting the mouth.
- Environmental allergens: Rarely, environmental allergens can cause mouth irritation.
Autoimmune Diseases
Certain autoimmune diseases can affect the mucous membranes of the mouth, causing widespread sores and inflammation. These conditions involve the immune system attacking the body's own tissues. Diagnosis requires specialized medical evaluation and testing.
- Pemphigus vulgaris: A severe autoimmune blistering disorder.
- Mucous membrane pemphigoid: Another autoimmune condition affecting the mucous membranes.
- Behçet's disease: A rare autoimmune disorder causing mouth sores and other symptoms.
What health issues cause mouth sores?
Mouth sores, also known as oral ulcers or canker sores, can be caused by a variety of health issues. The exact cause often remains unknown, but several factors are strongly linked to their development. These range from minor irritations to more serious underlying medical conditions. The severity and frequency of mouth sores can vary widely depending on the underlying cause.
Viral Infections
Many viral infections can manifest as mouth sores. Herpes simplex virus (HSV), the virus responsible for cold sores, is a common culprit. Other viruses, though less frequent, can also lead to ulcerations in the mouth. The sores associated with viral infections often have distinct characteristics, such as clustered blisters or a burning sensation prior to eruption. Early diagnosis and antiviral treatment are crucial in managing these infections effectively.
- Herpes simplex virus (HSV): Causes cold sores, typically appearing on the lips and surrounding areas.
- Hand, foot, and mouth disease (HFMD): A common viral infection, especially in children, presenting with mouth sores alongside rashes on the hands and feet.
- Other viral infections: A variety of less common viruses can also cause oral ulcerations.
Bacterial Infections
While less common than viral causes, bacterial infections can also result in mouth sores. These infections often arise from poor oral hygiene or weakened immune systems. The sores might appear as painful ulcers, often accompanied by other symptoms like bad breath or gum inflammation. Prompt treatment with antibiotics, in conjunction with improved oral hygiene, is crucial to prevent complications and promote healing.
- Poor oral hygiene: Allows bacteria to build up, leading to infections and sores.
- Weakened immune system: Makes individuals more susceptible to bacterial infections in the mouth.
- Specific bacterial species: Certain bacteria are more likely to cause oral ulcerations than others.
Nutritional Deficiencies
Deficiencies in certain vitamins and minerals, such as iron, vitamin B12, and folic acid, can increase susceptibility to mouth sores. These nutrients play a crucial role in maintaining the health of the oral mucosa. Ensuring adequate intake of these vitamins and minerals through a balanced diet or supplementation, under medical guidance, can help prevent or alleviate the issue. A blood test can confirm any deficiencies.
- Iron deficiency anemia: A common cause of mouth sores due to reduced red blood cell production.
- Vitamin B12 deficiency: Can result in various health problems, including mouth sores.
- Folic acid deficiency: Plays a crucial role in cell growth and repair, impacting oral health.
Autoimmune Diseases
Several autoimmune diseases can cause mouth sores as a symptom. Autoimmune disorders lead to the immune system attacking healthy tissues, including those in the mouth. Conditions such as Behçet's disease and Crohn's disease are known to be associated with recurrent and often severe oral ulcers. Managing these underlying conditions is crucial in controlling the frequency and severity of mouth sores.
- Behçet's disease: A chronic inflammatory disorder affecting blood vessels.
- Crohn's disease: An inflammatory bowel disease with various manifestations, including oral lesions.
- Other autoimmune disorders: Several other autoimmune conditions may present with mouth sores as a symptom.
Allergies and Irritants
Allergies and irritants can also trigger the development of mouth sores. Certain foods, dental products, or even acidic drinks can irritate the delicate lining of the mouth, leading to ulceration. Identifying and avoiding these triggers is crucial in preventing future occurrences. In some cases, an allergist may be consulted to pinpoint specific allergens.
- Food allergies: Reactions to certain foods can cause oral inflammation and sores.
- Dental products: Toothpastes, mouthwashes, and other products containing certain chemicals can irritate the mouth.
- Acidic foods and drinks: Frequent consumption can damage the oral mucosa.
What do autoimmune mouth sores look like?

Autoimmune mouth sores, often associated with conditions like Behçet's disease or lupus, can manifest in various ways, making definitive identification difficult without professional medical assessment. They often appear as recurrent ulcers, differing significantly from simple canker sores in their characteristics and persistence. Their appearance can range from small, shallow lesions to deep, painful, and potentially scarring ulcers. The size, shape, and location can vary widely, and they may or may not be accompanied by other symptoms, depending on the underlying autoimmune condition. The absence of a clear, easily identifiable pattern makes diagnosis challenging and necessitates a visit to a medical professional for accurate assessment and appropriate treatment.
Appearance of Autoimmune Mouth Sores
Autoimmune mouth sores can be quite variable in their appearance. They might present as single or multiple lesions, ranging in size from a few millimeters to several centimeters. Their color can vary from reddish-purple to yellowish-white, depending on their stage of healing. The borders may be well-defined or irregular, and the lesions may be shallow or deep. Importantly, they tend to recur frequently, often in the same location. Unlike simple canker sores which tend to heal within 7-10 days, these sores may persist for longer periods.
- Size and number: Can range from small, single ulcers to large, multiple lesions.
- Color: Often reddish-purple or yellowish-white.
- Shape and borders: Can be irregular or well-defined.
Location of Autoimmune Mouth Sores
The location of these sores can provide clues to their nature, although it is not always definitive. They can appear anywhere in the mouth, including the lips, gums, tongue, cheeks, and the palate. However, some autoimmune conditions might display a predilection for specific areas. For example, Behçet's disease often involves the mouth and genitals, while lupus can manifest in various locations, including the mouth, skin, and joints. Careful observation of the location and associated symptoms is crucial in diagnosis.
- Anywhere in the oral cavity: Lips, gums, tongue, cheeks, palate.
- Potential patterns: Some autoimmune diseases show preference for certain locations.
- Importance of location in diagnosis: Location, in conjunction with other symptoms, helps in proper diagnosis.
Pain and Other Symptoms
Pain is a common feature of autoimmune mouth sores. The severity of pain can vary significantly depending on the size and depth of the lesion. Some sores may be mildly uncomfortable, while others can be extremely painful, interfering with eating, drinking, and speaking. Beyond pain, other symptoms may include swelling, redness, and bleeding. These symptoms might be localized to the mouth or part of a wider systemic manifestation of the autoimmune disease.
- Pain: A characteristic symptom, varying in severity.
- Swelling and redness: Common signs of inflammation.
- Bleeding: May occur, especially with deeper ulcers.
Duration and Recurrence
A key distinguishing feature of autoimmune mouth sores is their tendency to recur. Unlike simple canker sores which usually heal within a couple of weeks, autoimmune lesions can persist for extended periods and reappear repeatedly. The frequency and duration of recurrences can vary considerably depending on the individual and the underlying autoimmune disease. Tracking the recurrence pattern can be helpful in diagnosis and monitoring disease activity.
- Extended healing time: Heal slower than canker sores.
- Recurrence: A hallmark of autoimmune mouth sores.
- Frequency and duration: Highly variable, depending on the underlying condition.
Differential Diagnosis
Because the appearance of autoimmune mouth sores can overlap with other oral lesions, a differential diagnosis is essential. It's crucial to rule out other conditions, such as aphthous ulcers (canker sores), oral herpes, oral thrush, and other infections or injuries. A thorough medical history, clinical examination, and potentially further investigations, such as blood tests or biopsies, are necessary to reach an accurate diagnosis and guide treatment.
- Requires ruling out other conditions: Can mimic other oral lesions.
- Need for thorough medical evaluation: History, physical exam, and possibly further tests.
- Importance of accurate diagnosis: Essential for appropriate management and treatment.
Why do I suddenly have sores all over my mouth?
The sudden appearance of sores throughout your mouth can be alarming, but several factors could be responsible. One common culprit is a viral infection, such as the herpes simplex virus (HSV), which causes oral herpes (cold sores). These typically present as small, painful blisters that can cluster together. Another possibility is a bacterial infection, perhaps stemming from poor oral hygiene. This can manifest as canker sores (aphthous ulcers), which are small, shallow ulcers that often appear on the inside of the cheeks, lips, or tongue. These can be triggered by stress, injury, or hormonal changes. Nutritional deficiencies, particularly those involving iron, vitamin B12, or zinc, can also contribute to mouth sores. A deficiency in these essential nutrients can impair the body's ability to repair damaged tissues, increasing susceptibility to sores. Less common, but still possible, is an allergic reaction. Certain foods, dental products, or medications can trigger an allergic reaction that leads to mouth sores. Finally, it’s important to rule out more serious conditions like hand, foot, and mouth disease (HFMD) in children or other less common infections. If your sores are severe, persistent, or accompanied by other symptoms like fever or fatigue, it is crucial to consult a doctor or dentist for proper diagnosis and treatment.
Are mouth sores contagious?
The contagiousness of mouth sores depends entirely on the underlying cause. Oral herpes, caused by the herpes simplex virus, is highly contagious and can spread through direct contact, such as kissing or sharing utensils. Hand, foot, and mouth disease (HFMD), also a viral infection, is equally contagious and spreads through contact with saliva, nasal secretions, or stool. However, most other causes of mouth sores, including canker sores and those related to nutritional deficiencies or allergic reactions, are not contagious. It's important to note that even if a particular type of mouth sore isn't inherently contagious, poor hygiene practices can still increase the risk of secondary bacterial infections, which can then be spread. If you suspect your mouth sores are caused by a contagious infection, practicing good hygiene, like frequent handwashing and avoiding close contact with others, is essential to prevent spreading the infection. Again, consult a healthcare professional for accurate diagnosis and advice on preventing contagion.
How long do mouth sores usually last?
The duration of mouth sores significantly varies depending on their cause and severity. Minor canker sores typically heal within a week or two, often disappearing without specific treatment. However, larger or more severe canker sores might persist for several weeks. Oral herpes sores usually last for 7-10 days, often going through stages of blister formation, ulceration, and crusting before healing. If the sores are caused by a more serious underlying condition like a bacterial infection or a systemic illness, they may persist for a longer period, and treatment might be necessary for resolution. The healing time also depends on factors like the individual's overall health, immune system function, and the effectiveness of any treatment administered. Persistent or recurring sores warrant medical attention to rule out any serious underlying health issues.
What home remedies can help soothe mouth sores?
While home remedies can provide temporary relief from the discomfort of mouth sores, they should not replace professional medical advice, especially if the sores are severe, persistent, or accompanied by other symptoms. Some common home remedies include rinsing your mouth with warm salt water several times a day to help clean the sores and reduce inflammation. Applying a topical anesthetic, like benzocaine gel, can help numb the pain. Avoiding acidic, spicy, or hard foods can minimize irritation. Staying well-hydrated is crucial for overall health and healing. Using a soft-bristled toothbrush and avoiding aggressive brushing can prevent further irritation. Over-the-counter mouthwashes with pain-relieving or antiseptic properties may also offer temporary relief. However, if your symptoms worsen or fail to improve after a few days with home remedies, it's essential to seek professional medical help for proper diagnosis and treatment to address the underlying cause of your mouth sores.

Deja una respuesta